Click on a title for the story
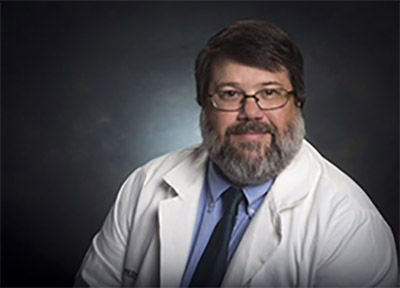
Lisa Morici, PhD is building the next generation of “Rockstar” Scientists at Tulane
(Pictured from left to right Erin Kuang, Allyson Hirsch, Lisa Morici, Madelyn Kist, and Sofia Santiago Torres.)
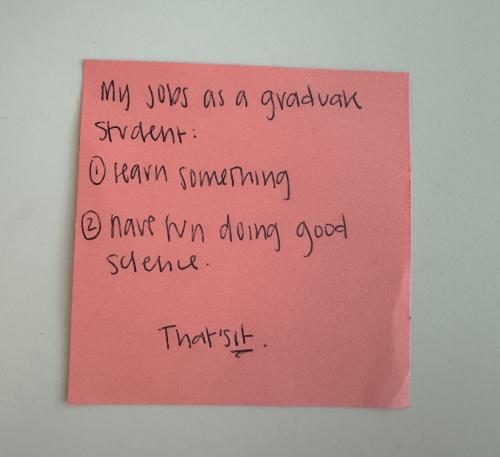
In a sunlit corner of the Morici Lab at Tulane University Medical School, a pink sticky note stands out with the message: “My job as a graduate student is to (1) learn something and (2) have fun doing good science. That’s it.” This simple yet powerful mantra, given as advice to Allyson Hirsch, a PhD student in Lisa Morici’s lab, reflects the ethos of Lisa Morici, PhD, a microbiologist and immunologist whose impact extends far beyond her own groundbreaking research. At Tulane, Dr. Morici is advancing microbiology and novel vaccine research while cultivating a new generation of innovators in her lab.
A self-described “hands-off” mentor, Morici refers to her team of trainees as “rockstars” and empowers them to live up to the title. Her lab is more than a hub of microbiological discovery—it’s a launchpad for future scientific leaders and entrepreneurs. Morici’s philosophy is straightforward: trust her students, give them autonomy, and be there when it counts. “I don’t have time to micromanage,” she says. “But I’m here when you need me.”
This approach promotes independence, resilience, and critical thinking - all essential for scientific and innovation success. Many PhD students and postdocs in Morici’s lab reported choosing Tulane Medicine for their research due to her strong reputation in the microbiology and vaccine community – both in academia and industry.
Her guidance has also supported the entrepreneurial journeys of two Tulane Innovation Institute teams: Rani Brooks, an Innovation Fellow, and founder of Biophoundry, and Kalen Hall, co-founder of Informuta. Both have participated in numerous TUII programs like Startup Team Mentoring, I-Corps, and Open Medical Innovation Challenge (Open MIC Night).
Brooks and Hall began their research careers in Morici's lab, where they were introduced to other expert faculty members through her extensive connections at Tulane. When Brooks needed expertise in synthetic biology, Morici facilitated a partnership with Nicholas Sandoval, a recognized authority in that field. Similarly, Hall benefited from Morici's introduction to DNA expert Zach Purcell. These initial academic collaborations laid a strong foundation for their startups, which later sought assistance from the Tulane Innovation Institute for further development. "I’m amazed at how the Tulane Innovation Institute has created opportunities for students interested in entrepreneurship and commercialization," Morici noted.
"Working with Lisa was one of the luckiest opportunities of my life. She is one of the most student-focused professors out there, consistently looking for ways to support her trainees. In my case, she provided lab space and some funding to help me start a project unrelated to her research focus. This early support enabled me to secure additional funding, allowing me to develop the preliminary work that has become the core of BioPhoundry. I could not have made it this far without her ongoing encouragement." Brooks said.
Rani Brooks also recalled Morici's altruistic efforts after Hurricane Katrina, when parts of New Orleans were still flooded and without power. She and other members of the Department of Microbiology and Immunology retrieved lab notebooks and documents to ensure that the work of many researchers would not be lost.
Morici is an accomplished scientist known for her ability to inspire young and aspiring researchers. Her current work is supported by the National Institutes of Health and the Department of Defense. She is developing a vaccine utilizing her adjuvant technology aimed at combating whooping cough, which has recently gained national media attention. The vaccine is anticipated to advance to Phase 1 clinical trials soon.
Together with her longtime colleague and best friend, James McLachlan, they are on the brink of a significant public health breakthrough. Both are dedicated to using science to benefit society and were recently honored with the IP Innovator Award at Tulane’s 2024 Research, Scholarship, and Artistic Achievement Awards. This award recognizes faculty members who advance patentable intellectual property with potential for licensing or commercialization.
What sets Morici apart is her holistic approach to mentorship. Beyond providing academic guidance, she fosters community, camaraderie, and well-being in her lab. "We're not just coworkers; we're friends and family," Allyson Hirsch stated, capturing the lab's close-knit culture. From celebrating personal milestones to supporting students through challenges, Morici creates an environment where individuals feel valued and supported.
She is known for helping students build valuable connections outside Tulane, often leading to significant career opportunities. “Lisa consistently connects me with key contacts, always endorsing me enthusiastically and mentioning my upcoming defense. Her introductions—at conferences, mixers, or meetings—have led to several informal job offers.” continued Hirsch. Former researchers frequently remain in touch, seeking her advice long after moving on to prestigious roles in academia and industry.
Her influence extends beyond the professional. "I've attended their weddings and sent baby gifts—these are lifelong connections," Morici shared, reflecting the deep, enduring relationships she maintains with her extended scientific family.
Morici's legacy is much more than academic achievements, published research, and the potential for intellectual property licensing; it is deeply rooted in the careers of the scientists she has mentored. While her guiding principle may be to "do good science," her true brilliance also lies in cultivating the next generation of scientific leaders who are poised to follow in her remarkable “rockstar” footsteps.

“Tulane was built to make the world a better place,” said Tulane University Provost Robin Forman at Open Season, a recent pitch competition event hosted by the Tulane Innovation Institute, where the recipients of the latest round of the Provost’s Proof of Concept (PPOC) fund were also announced.
The university has addressed pressing health challenges since its founding in 1834 to combat yellow fever and cholera in New Orleans. This legacy continues through initiatives like PPOC, which supports innovators in finding solutions to modern global issues.
In this fourth round of the PPOC fund, managed out of the Robert L. Priddy Innovation Lab at the Tulane Innovation Institute, three new recipients carried on Tulane’s mission of empowering our community to solve world problems. They were awarded $50,000 each for projects that could redefine healthcare and environmental science in the marketplace.
Chandler Monk, MS, who is a researcher in our department's Zwezdaryk lab was awarded this honor for her proposal on use of CRISPR technology to create a quick and affordable test for detecting cytomegalovirus. This virus is a significant cause of congenital disabilities and health problems. Unlike traditional lab tests, her isothermal test can be used in clinics or remote locations, helping to make early treatment available to people worldwide.
Tulane virologist named National Academy of Inventors Fellow
December 10, 2024 9:01 AM | Keith Brannon kbrannon@tulane.edu
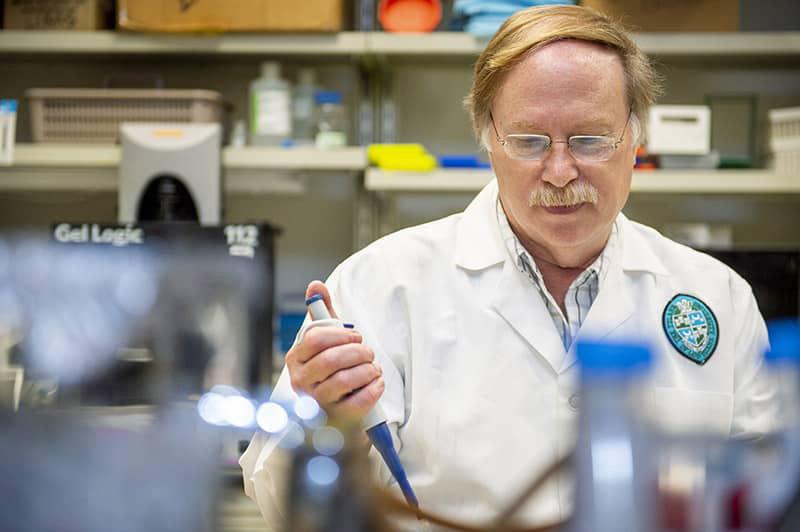
Renowned Tulane University virologist Robert Garry has been named a fellow of the National Academy of Inventors (NAI) for his groundbreaking work finding new treatments and diagnostics to fight infectious diseases like Lassa Fever, Ebola, influenza and other global threats over the past four decades.
Being named an NAI Fellow is one of the highest professional distinctions awarded solely to inventors.
“I'm very honored to be nominated and chosen,” Garry said. “You don't get this kind of recognition that often. It is a high honor.”
Garry, professor of microbiology and immunology at Tulane University School of Medicine, holds 25 patents for innovations against infectious diseases. He worked with other Tulane scientists to start a Lassa fever program in West Africa and now manages a consortium of researchers who are developing countermeasures — including diagnostics, immunotherapeutics and vaccines — against diseases including Lassa virus, Ebola and Marburg viruses and other high-consequence pathogens. His work includes developing a treatment and prevention using cloned antibodies from Lassa fever survivors.
"Bob Garry is a globally recognized leader in the battle against today’s greatest threats to public health,” Tulane President Michael A. Fitts said. “With quiet determination and humility, he relentlessly pursues the causes and cures for both long-known infectious diseases as well as new and emerging and perils.”
The Lassa treatment, which Garry developed with Tulane virologist James Robinson, MD, could move into clinical trials next year. He has also developed rapid testing kits for Lassa and other infections as well as peptide-based therapies against viruses. Garry has published more than 250 papers in virology, with cover stories in top journals, including Nature and Science.
“Throughout his 40 years at Tulane, Bob Garry has built a global reputation as an ambitious, rigorous and creative researcher, a highly sought after collaborator, a dedicated mentor, and a beloved colleague. I am absolutely thrilled to see him recognized by the NAI for his many innovative and impactful contributions to our fight against some of the most challenging infectious diseases,” said Tulane Senior Vice President for Academic Affairs and Provost Robin Forman.
Garry is one of 170 individuals named as 2024 NIA Fellows. Honorees represent 39 U.S. states, 12 countries, and 135 research universities, governmental and non-profit research institutions worldwide.
The 2024 Class of Fellows will be honored and presented their medals by a senior official of the United States Patent and Trademark Office at the NAI 14th Annual Meeting in Atlanta next June.
“This year's Class of NAI Fellows represents a truly impressive caliber of inventors. Each of these individuals are tackling real-world issues and creating solutions that propel us into the future. Through their work, they are making significant contributions to science, creating lasting societal impact, and growing the economy,” said Dr. Paul Sanberg, FNAI, President of the NAI. “NAI Fellows as a whole are a driving force of innovation, generating crucial advancements across scientific disciplines and creating tangible impacts as they move their technologies from lab to marketplace.”
Since its founding in 2012, the NAI Fellows program has grown to include 2,068 exceptional researchers and innovators, who hold over 68,000 U.S. patents and 20,000 licensed technologies. NAI Fellows are known for the societal and economic impact of their inventions, contributing to major advancements in science and consumer technologies. Their innovations have generated over $3.2 trillion in revenue and generated 1.2 million jobs.
Owl Club Awards honor teaching excellence at Tulane School of Medicine

Kerstin Honer Zu Bentrup, PhD, Associate Professor, Microbiology & Immunology (Photo by Carolyn Scofield)
Owl Club Awards honor teaching excellence at Tulane School of Medicine
The Owl Club is the student organization for academic excellence at Tulane University School of Medicine. Owl Club representatives compile evaluations and feedback from every course taught, and present teaching awards to top faculty every spring. Congratulations to this year’s Owl Club Award winners!
T1 Best Integrated Module:
Endocrine/Reproduction (Brian Rowan, MD)
T1 Course of the Year:
Gross Anatomy (Samir Anadkat, MBBS, MS)
T1 Best CBL/TBL Facilitator:
David Franklin, PhD
T1 Professor of the Year
Samir Anadkat MBBS, MS
Highest average review scores T1 Lecturers:
David Franklin, PhD
Samir Anadkat, MBBS, MS
T. Cooper Woods, PhD
T2 Best Integrated Module:
Cardiovascular (Elma LeDoux, MD)
T2 Course of the Year:
Brain, Mind, and Behavior (Elizabeth Crabtree, MD; Ashley Weiss, DO; David Blask, MD, PhD; Norm Kreisman, PhD; and Adam Lawson, PhD)
T2 Best CBL/TBL Facilitator:
Kerstin Honer zu Bentrup, PhD
T2 Innovation Award:
Elizabeth Crabtree, MD
T2 Professor of the Year:
Kerstin Höner zu Bentrup, PhD
Click for a list of all the winners.
April 07, 2023 9:30 AM | Keith Brannon kbrannon@tulane.edu
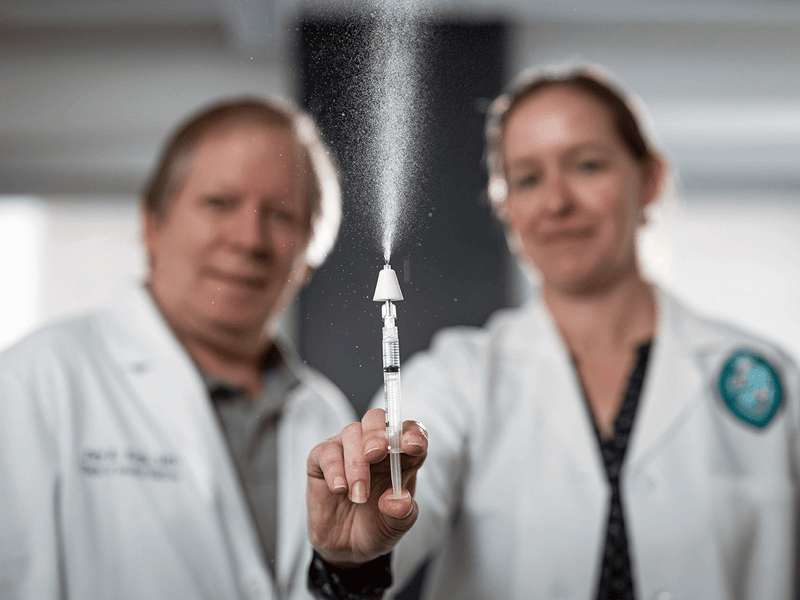
The new vaccine, called CladeVax, is a nasal spray designed to efficiently target mucosa in the nose, throat and lungs to protect the area most at risk for infection from the antibiotic-resistant Klebsiella pneumoniae bacteria, a leading cause of pneumonia. Photo by Rusty Costanza
The National Institute of Allergy and Infectious Diseases awarded a contract worth up to $16 million to Tulane University to bring a nasal spray pneumonia vaccine to Phase One clinical trial. University researchers invented the experimental vaccine to thwart antibiotic-resistant Klebsiella pneumoniae, a leading cause of bacterial pneumonia...As doctors try to find new types of antibiotics to fight these so-called superbugs, Tulane University School of Medicine researchers Elizabeth Norton, PhD, and Jay Kolls, MD, inventors of the experimental Klebsiella pneumoniae vaccine, are working to protect people before they are exposed to the pathogens in the first place.
Read more about this potentially life-saving research being conducted at Tulane University.
No, mRNA Vaccines Aren’t Widely Used in Livestock and Can't Get Into the Food Supply
By Tom Kertscher
January 23, 2023

Cattle occupy a feedlot in Columbus, Neb., on June 10, 2020. (AP)
Experts said there is no widespread use of mRNA vaccines in livestock in the United States.
And even in cases in which mRNA vaccines are used in livestock, there is no chance those vaccines could transfer to a person who eats meat from a vaccinated animal, according to the experts.
...Tulane University professor Robert Garry, whose research specialties include virology, said there is no widespread injection of mRNA vaccines into livestock.
..."there is no chance that a veterinary mRNA vaccine would produce any protein in a person consuming the meat from a vaccinated animal," Garry said.
Read the complete article about this contentious topic.
Tulane Researchers Helping Develop Fentanyl Vaccine
WDSU Reporter: Elizabeth Kuebel
Researchers at Tulane School of Medicine are helping develop a potentially life-saving vaccine. It would target the synthetic opioid fentanyl.
Dr. Elizabeth Norton is among the Tulane researchers that have been collaborating with ones in Texas. She even helped create a special piece of the vaccine in New Orleans.
Click this link or the picture to view the entire interview.
Tulane Researchers to Develop New Lyme Vaccine with Lasting Protection
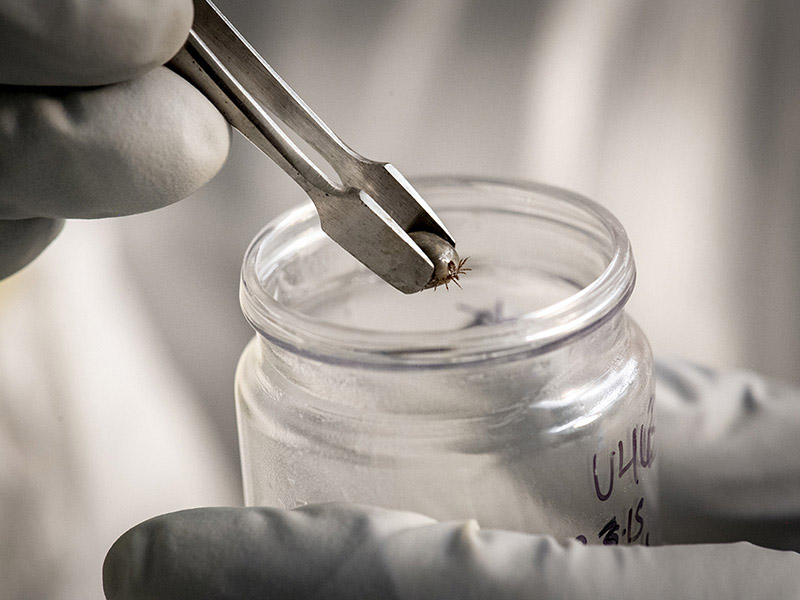
The nonhuman primate model of Lyme disease is only available at the Tulane National Primate Research Center, and Monica Embers, Ph.D., has long been at the forefront of new Lyme diagnostics, preventatives, and treatments.
Cases of Lyme disease are rising across the globe, yet there is still no vaccine on the market to protect people against the tick-borne infection. The nonhuman primate model of Lyme disease is only available at the Tulane National Primate Research Center, and Monica Embers, Ph.D., has long been at the forefront of new Lyme diagnostics, preventatives, and treatments. Click to read more about this important research.
NIH advisers urge tighter oversight of experiments on deadly viruses

A worker carries disinfecting equipment outside the Central Hospital of Wuhan in China in February 2021. (Ng Han Guan/AP)
Robert Garry, a virologist at Tulane University, said he would support a ratcheting up of biosafety requirements for certain experiments...“We’re not opposed to the regulations. We need to know what the rules are. But don’t shut us down,” Garry said. “This work needs to be done.” Read more in this washingtonpost.com article discussing researchers' thoughts on continuing investigation of COVID and many other diseases.
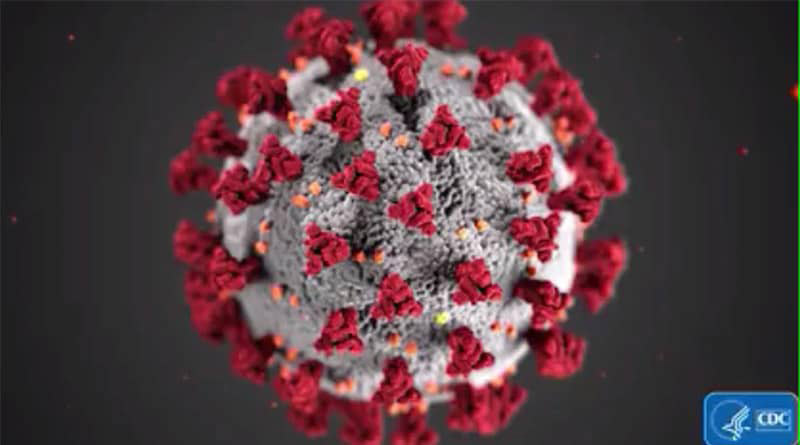
Study Finds Wuhan Market as Likely Origin of COVID-19 Pandemic
Robert Garry, professor of microbiology and immunology at Tulane University School of Medicine, explains how a team of leading virologists traced the origins of COVID-19. Read more of Dr. Garry's observations and study of the virus. Video by Roman Vaulin.
Why This 'Very, Very Contagious' Coronavirus Subvariant Is Causing Cases To Rise Again
By Nina Golgowski
May. 5, 2022, 09:55 AM EDT | Updated 4 hours ago
The omicron subvariant BA.2.12.1 is poised to be the next dominant strain in the U.S. Mutations appear to have helped it replicate better and resist prior immunity.
...The current seven-day rolling average of cases is back to where it was in February, with an average of 64,000 cases tallied Monday by the Centers for Disease Control and Prevention. That’s roughly three times what it was toward the end of March...Deaths from COVID-19 have stayed near record lows.
This drop in fatalities is likely thanks in part to current dominant variants appearing to be less deadly and vaccination rates being high in the U.S., Dr. Robert Garry, a professor of microbiology and immunology at Tulane University, told HuffPost. As of this week, roughly 66% of the U.S. population has been fully vaccinated, according to the CDC. Click to read more scientific evidence on this ever-evolving virus.
Virus Mutations Aren’t Slowing Down. New Omicron Subvariant Proves It.
Story By Joel Achenbach
May 1, 2022|Updated May 1, 2022 at 5:00 p.m. EDT

...The coronavirus, SARS-CoV-2, has had billions of chances to reconfigure itself as it has spread across the planet, and it continues to evolve, generating new variants and subvariants at a clip that has kept scientists on their toes. Two-and-a-half years after it first spilled into humans, the virus has repeatedly changed its structure and chemistry in ways that confound efforts to bring it fully under control...
“This virus has probably got tricks we haven’t seen yet,” virologist Robert F. Garry of Tulane University said. “We know it’s probably not quite as infectious as measles yet, but it’s creeping up there, for sure.” Click to read the entire Washington Post article.
NIH Orders Sweeping Review of Potentially Risky Experiments on Viruses and Other Pathogens
By Joel Achenbach
March 1, 2022 at 5:20 p.m. EST

...Biosecurity and biosafety in scientific research have been intensely controversial topics for years. A decade ago, the debate raged over the publication of research on influenza viruses, which some scientists feared could be used by hostile actors to create a bioweapon....
The newly posted scientific papers should end debate about where the pandemic began, said Robert F. Garry, a Tulane University virologist who was a co-author on both papers as well as the 2020 Nature Medicine report.
“It pretty much screws the lid on it as far as I’m concerned,” said Garry, who has been among the most vocal opponents of the lab leak speculation. Click to read the entire article.
Studies Offer Further Evidence That the Coronavirus Pandemic Began in Animals in Wuhan Market
By Katherine Dillinger, CNN
Updated 9:09 AM ET, Sun February 27, 2022
The findings are "as close to having the virus in an animal as you can get," Robert Garry, a professor of microbiology and immunology at Tulane Medical School, told CNN.
Garry was co-author on the study that found at least two zoonotic or animal-transmission events. It notes that the pandemic began with two major viral lineages, called A and B, although it says there were probably even more forms of the virus "that failed to establish in humans." Lineage B is the more common of the two and the only one that had previously been found at the market, but the study says lineage A was also circulating around the area early in the outbreak. Click to read the entire story on CNN.com.
DeSantis Wars with Biden's FDA Over Monoclonal Antibodies Decision
Florida Gov. Ron DeSantis, a major supporter of monoclonal antibody treatments for COVID-19, is going to war with the Biden administration over the Food and Drug Administration's revocation of authorization for two antibody cocktails found to be ineffective against the omicron variant.
...“The antibody doesn't do what it's supposed to do anymore,” said Dr. Robert Garry, an immunologist at Tulane University School of Medicine. “The unfortunate thing is this virus is spreading around to literally millions of people, and that gives it the opportunity to come up with these mutations — and it's going to render drugs like these monoclonal antibodies useless in some cases.”...“The FDA is not going to come in — and shouldn't in my opinion … leave drugs on the market that don't work. And it was an emergency use authorization too. They specifically do that for reasons like this,” Garry said. Click to read the entire Washington Examiner article
There’s a New Version of Omicron But So Far It Doesn’t Appear To Be More Dangerous
As a new version of the highly contagious omicron variant of the coronavirus spreads in parts of Asia and Europe, the World Health Organization recommended Monday that officials begin investigating its characteristics to determine whether it poses new challenges for pandemic-weary nations.
...“Variants have come, variants have gone,” said Robert Garry, a virologist at Tulane University School of Medicine. “I don’t think there’s any reason to think this one is a whole lot worse than the current version of omicron.” Read the entire Washington Post article.
Doctor Says Evidence is Clear - Boosters Help Against Omicron
“We're seeing 70, 80 percent effectiveness, depending on the study that you look at, which is just, it really is mind blowing at how well the vaccines are working." --Dr. Lisa Morici

Author: Meg Farris (WWL)
Published: 5:24 PM CST January 13, 2022
Updated: 5:24 PM CST January 13, 2022
NEW ORLEANS — We've been hearing from some of you asking, “Why get a COVID vaccine if it doesn't work against the Omicron variant.”
So what is the science behind breakthrough cases and what does and doesn’t work?
First, here's where you can find the latest vaccine science. Type in Google Scholar. Click on that search engine then type in the topic you're looking for. You'll have access to the first-hand, scientific studies that are not filtered through websites with an agenda, social media, or even rewritten by a journalist.
Understanding Omicron’s Many Mutations
The virus’s spikes have far more changes than we’ve seen in any previous variant, and researchers are racing to figure out how they affect it — and us
The omicron variant of the coronavirus has about 50 genetic mutations, and a whopping 36 of them are in the all-important spike. That is the part that lets the virus attach to human cells and worm its way inside.
Scientists are not sure exactly what this area’s function is, said Tulane microbiologist Robert F. Garry, an expert on the virus’s anatomy. It may help viruses attach to cells in some way. Read more about the virus and Dr. Garry's comments in this Washington Post article.
We All Want the Omicron Variant to be Milder. Here's Why It's Too Soon to Know
Robert Garry, virologist and immunologist at the School of Medicine, says assuming that a portion of the genetic material of the Omicron variant came from a common cold virus “probably would not make it more like the common cold virus.” Read more about the Omicron Variant.
Key threat to unvaccinated people is other unvaccinated people

A counterintuitive claim about COVID-19 argues that people who are not vaccinated actually face a bigger threat from vaccinated people than from the unvaccinated.
...The claim "is wrong — dangerously so," said virologist Robert Garry, professor at the Tulane University School of Medicine.
"Unvaccinated people are most likely to spread to other unvaccinated people," he said. The next most likely pattern is unvaccinated people spreading to vaccinated people, he said. Read more of Dr. Garry's comments here.
Wuhan, U.S. Scientists Planned to Make Coronaviruses, Documents Leaked by DRASTIC Show

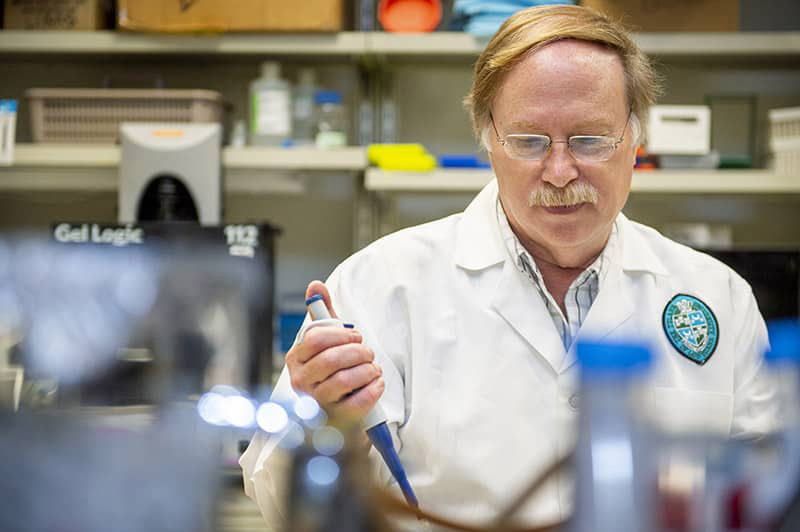
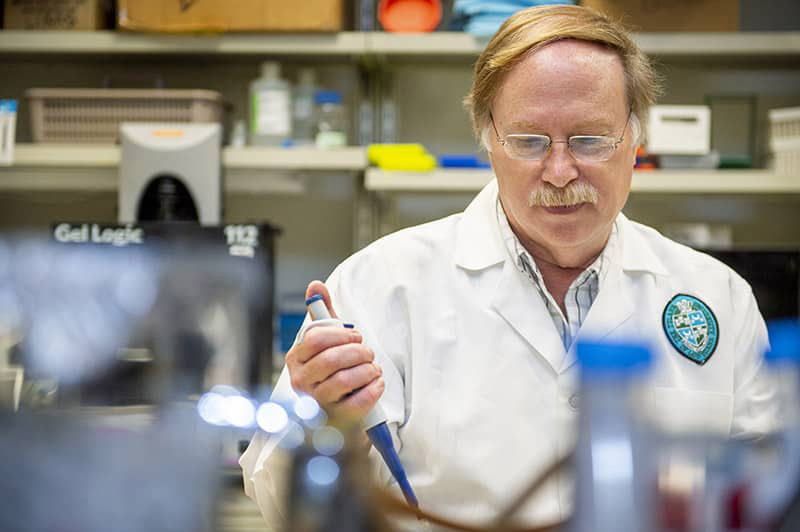
Tulane Microbiology Professor Robert Garry, PhD. Photo by Paula Burch-Celentano.
Article By Ed Browne - Newsweek.com
"...other scientists Newsweek spoke to disputed this interpretation..." implied by the title of this article.
"Robert Garry, a doctor of microbiology and a virology researcher at the Tulane University School of Medicine in Louisiana, said: "What they are proposing to do here is reconstitute [reconstruct] bat viruses related to SARS-CoV-1 [the viruses that causes SARS] already found in nature, not create a new virus genome... You certainly could not have generated SARS-CoV-2 [the virus that causes COVID] this way." Read more of Dr. Garry's comments here.
Did the Coronavirus Jump from Animals to People Twice?

A preliminary analysis of viral genomes suggests the COVID-19 pandemic might have multiple animal origins — but the findings still have to be peer reviewed. Tulane School of Medicine's Dr. Robert Garry shares his thoughts on this matter. Read about the possibility here.
Ebola Might Linger In Survivors And Could Trigger Outbreaks Years Later, Scientists Warn

GETTY IMAGES
It’s not clear how Ebola virus is able to persist in the body or what leads it to reactivate later on, according to Tulane Medical School professor Robert Garry. Learn more about this discovery
Who needs a COVID vaccine booster shot and when should they get it?
When will we need a booster? Is it free? What are the expected symptoms? It may be necessary for most Americans to get another dose of a COVID-19 vaccine soon. Right now, Moderna and Pfizer are offering so-called "boosters" to people with certain medical conditions, but what does that mean for the rest of us? Tulane University's Dr. Lisa Morici gives her expert opinion on the answer to that question. Read what she said here.
How the Delta Variant Differs: A Virologist's Point-of-View
Tulane scientist says one of the variant’s mutations allows the virus to replicate at high levels
Since the fourth surge in COVID-19 infections began, we have heard a lot about how the Delta variant of the novel coronavirus is different from the original virus and a Tulane University virologist explains how. Click to read more.

Peter Daszak (right), Thea Fischer (left) and other members of the World Health Organization team investigating the origins of covid-19 arrive at the Wuhan Institute of Virology in Wuhan in China's central Hubei province on Feb. 3. (HECTOR RETAMAL/AFP VIA GETTY IMAGES)
Once dismissed as a conspiracy theory, the idea that the covid virus escaped from a Chinese lab is gaining high-profile attention. As it does, reputations of renowned scientists are at risk — and so is their personal safety.
At the center of the storm is Peter Daszak, whose EcoHealth Alliance has worked directly with Chinese coronavirus scientists for years. Click to read more.
Covid variant from India a concern but you should be good with vaccine
A local microbiologist said that with the vaccine, even if you get the variant, it should protect you from severe consequences.
Author: Meg Farris (WWL)
Published: 5:22 PM CDT May 11, 2021
Updated: 5:22 PM CDT May 11, 2021
NEW ORLEANS — The World Health Organization is reclassifying the COVID variant spreading in India as a “variant of concern” at the global level. The triple-mutant COVID variant is highly contagious. Click to read more.
You should get vaccinated, even if you've had COVID - Here's why
The mRNA technology in the two-dose vaccines gives us better, more consistent protection than the virus does.
Author: Meg Farris (WWL)
Published: 5:23 PM CDT April 27, 2021
Updated: 5:43 PM CDT April 27, 2021
NEW ORLEANS — If you've decided that you don't need a COVID vaccine because you were infected with the virus in the past, some new information may change your mind. Immunity from the COVID vaccine versus immunity from the COVID natural infection: which protects better? We're finally getting answers from science. Tulane Microbiology and Immunology expert Dr. James McLachlan, helps us sort out a study from the University of California Irvine. Click to learn more.
CDC recommends resuming use of J&J COVID-19 vaccine; Tulane vaccine expert weighs in
NEW ORLEANS (WVUE) - A panel of advisers to the CDC recommends that COVID-19 vaccinations with the Johnson & Johnson vaccine resume in the U.S. And a Tulane University vaccine researcher says she trusts the experts’ making the recommendation and thinks the public should have confidence in the recommendation. Read More.
The J&J vaccine - local doctor answers your questions
Author: Meg Farris (WWL)
Published: 5:17 PM CDT April 13, 2021
Updated: 5:17 PM CDT April 13, 2021
The CDC's vaccine advisory committee is meeting Wednesday to see if there is a possible link between the Johnson & Johnson vaccine and rare blood clots.
We know many of you have gotten that same vaccine, so here are some answers to your questions, from Tulane vaccinologist Dr. Lisa Morici. Click to read the questions and Dr. Morici's answers.
VAX Facts: 4 big questions concerning the vaccine
NEW ORLEANS — The demand for getting a COVID vaccine in Louisiana is going down. The state ranks in the bottom six when it comes to the percentage of people vaccinated.
We understand that you may still have some questions about the shot, so we got some answers to your most asked vaccine questions.
For our answers we turn to Tulane Vaccinologist Dr. Lisa Morici: Click to learn more about the COVID-19 shot.
‘Double mutant’ COVID strain discovered in California
NEW ORLEANS (WVUE) - Variants of the novel coronavirus are teaming up, so to speak. A so-called “double mutant” is making headlines.
Dr. Bob Garry is a Tulane University virologist and microbiologist who reacted to the two mutations found in one virus.
“This one has two mutations that we’ve been looking at for a while and they are in some important parts of the molecule that lets the virus attach to cells, so we have to keep an eye on them,” said Garry. Click to view the video of Dr. Garry's interview by Sabrina Wilson on Fox 8 Local First and read what else Dr. Garry had to say.
Lab leak Covid-19 theory is like something out of a comic book, virologist says
..."That's the way it would be in a movie or some sort of a thriller or a comic book," retorts Garry, who studies viruses in the field and in the lab and who helped write a study published in March of last year that showed the virus arose naturally. Click to read this article
WHO report finds coronavirus probably emerged in bats, 'extremely unlikely' to be result of lab leak
...Robert Garry, a virologist at Tulane University School of Medicine who wasn't involved with the WHO investigation, said the research team was right to largely dismiss the idea that the virus leaked from a lab. Click to read the entire article,
Vaccines are Safe Despite Review of COVID Shot Not Available in U.S., doctor says.
The AstraZeneca COVID vaccine is under review in some European countries but that shouldn't stop people from getting shots here, doctor says.
Author: Meg Farris (WWL)
Published: 5:23 PM CDT March 16, 2021
Updated: 5:53 PM CDT March 16, 2021
NEW ORLEANS — In February, preliminary science showed the AstraZeneca COVID vaccine was safe, giving 100 percent protection against severe illness.
Now it's under further investigation in Europe, after 37 cases of blood clots, out of the 17 million people who had been vaccinated.
So what does this mean if you're trying to decide about getting vaccinated?
A number of European countries are temporarily pausing the use of the AstraZeneca COVID vaccine after reports of dangerous blood clots in some people. That vaccine is not yet approved in the U.S., but reports can cause fear about the current vaccines. So we asked Tulane Vaccinologist Dr. Lisa Morici for the vax facts.
“At this point, there's no causal relationship between any of the vaccines and serious adverse events,” said Dr. Lisa Morici, who is in the Tulane Department of Microbiology and Immunology.
Dr. Morici reminds us that millions of people are being vaccinated across the globe. Blood clots can occur for many reasons. The important question to ask now is, is it happening more frequently in people who got the vaccine?
“Right now the reports are that the number of cases are no higher than what you would typically expect in your everyday population,” she explained.
You may remember warnings were announced about reactions in people who have pre-existing severe allergies. There were a few cases in a million. Those are treatable. For now, doctors will carefully examine the new cases of blood clots.
When asked, as an expert, if she trusts the system that's in place to find and report any link to the vaccine, she replied, “I do. There are numerous mechanisms in place for monitoring the safety of these vaccines.”
The concern is, if enough people globally don't get vaccinated, the coronavirus could then infect many, and mutate, causing new variants. She says catching the virus should be feared more than the vaccines.
“Thousand times greater chance of dying from COVID than from getting the vaccine, even if the vaccine could cause death.”
The data from the AstraZeneca vaccine trial in the U.S. should be ready soon, and will be studied very carefully for safety before it is authorized for emergency use.
Thursday, The European Union’s drug regulatory agency will review the findings on the AstraZeneca vaccine and decide if action needs to be taken.
Some Scientists Question W.H.O. Inquiry Into the Coronavirus Pandemic’s Origins

Tulane Microbiology Professor Robert Garry, PhD. Photo by Paula Burch-Celentano.
Article By James Gorman - New York Times
A small group of scientists and others who believe the novel coronavirus that spawned the pandemic could have originated from a lab leak or accident is calling for an inquiry independent of the World Health Organization’s team of independent experts sent to China last month.
While many scientists involved in researching the origins of the virus continue to assert that the SARS-CoV-2 pandemic almost certainly began in a leap from bats to an intermediate animal to humans, other theories persist and have gained new visibility with the W.H.O.-led team of experts’ visit to China. Officials with the W.H.O. have said in recent interviews that it was “extremely unlikely” but not impossible that the spread of the virus was linked to some lab accident....Click to read the entire article.
Tulane Professor Robert Garry, PhD was quoted in this New York Times article
Robert F. Garry, a virologist at Tulane University Medical Center, recently posted on the website Virological a report that is not yet peer-reviewed that described new evidence that aspects of the virus that seemed unusual at first had been found in new viruses in Japan, Thailand and Cambodia. He and his co-authors concluded, “These observations are consistent with the natural origin of SARS-CoV-2 and strongly inconsistent with a laboratory origin.”
He said that he was familiar with some of the views of the letter signers expressed in previous media appearances or on social media, involving speculation about ways the virus could have come from laboratory work, and that none of those views appeared in the letter.
Dr. Garry said the possible scenarios described in the letter were that “the Wuhan Institute of Biology either had SARS-CoV-2 or something very close to it before the outbreak. And for whatever reason, some grand conspiracy, they just didn’t want to tell anybody about it.”
Scientists Narrowing in on Virus Origin
Scientists are getting closer to discovering the origins of the novel coronavirus that sparked the pandemic.
"We've been studying the origin of viruses for a long time," said Dr. Robert Garry, a virologist at Tulane University School of Medicine, who is something of a disease detective.
He and his team have been looking for coronaviruses in Southeast Asia mostly in bats to see if they can find the progenitor of the virus that causes COVID-19.
Dr. Garry said his team has found several close relatives and are close to finding the virus’ direct ancestor.
"By comparing these viruses, looking for different signatures - we call them signature motifs, different parts of the virus proteins - we can start to piece together how a virus like SARS-CoV-2 could have evolved," he explained.
"We need to find out what other SARS-like viruses are out there so we can be much better prepared the next time. We don’t want another pandemic like this to happen."
As an expert in the origin of viruses, Dr. Garry said there is no truth to the conspiracy theories that the novel coronavirus may have been created in a lab as a bio weapon.
"There’s no reason to think that investigators in China had any viruses anywhere close to SARS-CoV-2 or knew about it before the outbreak happened."
VAX Facts: Rising questions on the after-effects of the COVID vaccine
Author: Meg Farris (WWL)
NEW ORLEANS — We were curious about some stories that came out in the news after people were vaccinated against COVID.
One was why did Mayor Cantrell have a positive test after her vaccine. And another is why do some people still get a mild case after being fully vaccinated.
Last week Mayor LaToya Cantrell was denied access to the White House after getting a positive result from a coronavirus test.
“Upon taking that, they gave me a call and said that I had tested positive and I'm like, ‘Oh no, I've never tested positive,’” Mayor LaToya Cantrell said.
Shortly afterward she had two more tests that were negative. She had just gotten her first dose COVID vaccine two days earlier. Did that make a difference?
“Getting the vaccine will not give you a false positive test,” said Dr. Bob Garry, Tulane Microbiologist and Immunologist.
Dr. Garry said the PCR tests the mayor had are more than 98 percent accurate. He suspects it was a false positive.
“This apparently is what happened to the mayor. She just happened to be in that unlucky one percent where the test gave a false result,” he explained.
Another question is why are we seeing headlines like the one out of Oregon, where four people tested positive and some have mild symptoms after full vaccine immunity? We know the vaccine does not give you the virus, and the current ones are 95 percent effective.
“That is not 100 percent. You know five people out of 100 are going to get infected and there, the vaccines are going to keep you from getting a severe illness,” said Dr. Garry.
So the vaccines will not necessarily keep you from getting infected when you're exposed to the virus.
“You might just replicate the virus enough to make the test come up positive, but you're either going to be asymptomatic or have very mild illness.”
“Hopefully, when all of us get the vaccine and we drive this virus into the ground, you know, then there won't be a need for masking and social distancing anymore,” said Dr. Garry.
And with vaccine supplies ramping up, that could come sooner than later.
The PCR COVID test that the mayor had is not the rapid test, which is not quite as accurate as the PCR test.
Mardi Gras 2020 Spawned up to 50K Coronavirus Cases...

People throw beads from a balcony on Royal Street during Mardi Gras in the French Quarter in New Orleans, Feb. 25, 2020
Staff Photo by Sophia Germer for Nola.com
Public health officials have largely accepted that last year's Mardi Gras helped make New Orleans an early coronavirus hotspot in the U.S., even if a lack of testing made it hard to be sure.
But a new study that sought to pinpoint how the virus spread through the city has found that 2020 Carnival revelry was responsible for tens of thousands of coronavirus cases, after a single person likely brought it to New Orleans in the weeks before Mardi Gras.
Researchers at the Scripps Research Institute, Tulane University, LSU Health Shreveport and several other institutions said in a pre-publication report released Monday that the coronavirus probably arrived in New Orleans about two weeks before Fat Tuesday, likely from a person traveling from Texas.
Follow this link to learn more about how Mardi Gras 2020 spawned up to 50K Coronavirus Cases
Virus Hunter: 'We Have to Double Down' to Fight COVID-19 Variants

Tulane Microbiology Professor Robert Garry, PhD. Photo by Paula Burch-Celentano.
The SARS-CoV-2 virus is rapidly evolving as COVID-19 spreads across the globe. Tulane Microbiology Professor Robert Garry, PhD, is part of a national team of leading virologists who are sequencing coronavirus samples to monitor mutations. He spoke with Tulanian Now about what the new variants mean for transmission and how they may impact the next phase of the pandemic.
Q: What do we need to know about the new COVID-19 variants?
Robert Garry: We have three or four variants now circulating around the world. The one that most people recognize is the United Kingdom variant, known as B.1.1.7. It spreads easier than the other variants, but it is not more pathogenic. It doesn’t cause increased symptoms or illness. And, so far, there is no evidence it causes increased deaths. Now, the fact that you've got it spreading easier, means you're going to have more people infected. And that ultimately will result in more people in the hospital and more deaths. But, individually speaking, if you're infected with that variant, it's no worse than the ones that are currently most prevalent.
Q: How common is the U.K. variant in the United States right now and do you expect it to become the dominant strain here?
It is not prominent yet. We don't have good numbers, unfortunately, because the United States is behind other countries in terms of the amount of sequencing that we’re doing. Once it gets a toehold in, it will start to take off. But that's going to take several weeks to several months.
Q: Should we change our behavior because of the new variant?
Yes. We have to double down on those protections that everybody has been talking about — social distancing and wearing a good mask. Wear the best mask you can. If you can get your hands on a KN95 or an N95 that’s properly fitted, that's the kind of mask you want to wear. If you can't get one of those, multiple layers of cloth will do in terms of keeping the virus out of your lungs and keeping you from expelling it to other people so they can’t get infected.Follow this link to learn more about the continuing pandemic straight from Dr. Robert Garry, a respected Tulane researcher.
BioAesthetics and Tulane Awarded Grant to Develop New Advanced Wound-Care Graft

BioAesthetics’ founder and CEO Nick Pashos, PhD, and Lisa Morici, PhD, associate professor of microbiology and immunology at Tulane University School of Medicine.
The National Science Foundation has awarded a $250,000 grant to BioAesthetics Corp. to develop a new advanced wound-care product for treating bed sores or pressure ulcers. The product will be tested at Tulane University.
The Small Business Technology Transfer (STTR) Phase I award will fund initial testing and development of a skin graft that combines the company’s tissue regeneration technology with infection-fighting drugs to better promote healing. Follow this link to learn more about this advanced wound-care product.
What We Know About COVID-19 Immunity
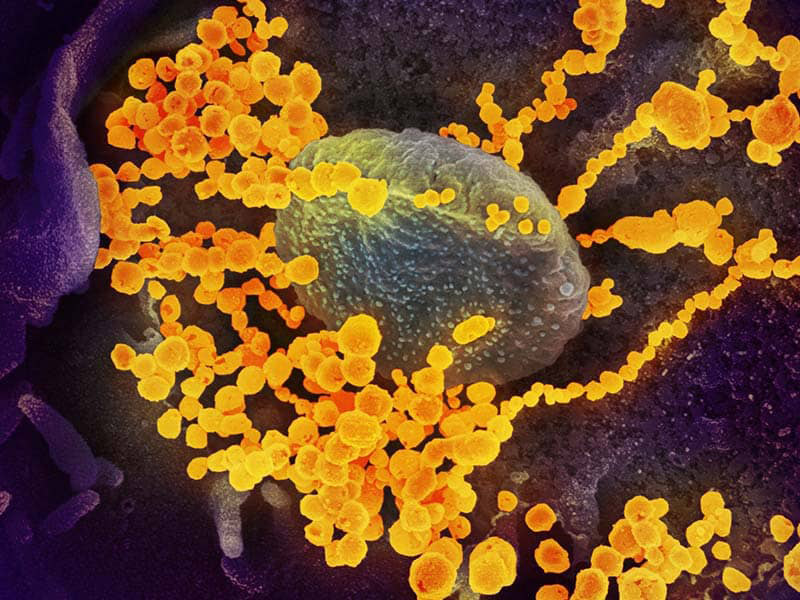
Electron microscope image of SARS-CoV-2 (round gold objects) emerging from the surface of cells cultured in the lab. Image courtesy of the National Institute of Allergy and Infectious Diseases.
Are people likely to catch COVID-19 twice? How long can immunity last? Why do some survivors develop antibodies from SARS-CoV-2 while others seemingly don’t?
These are just some of the questions scientists are still working to answer almost seven months into the global COVID-19 pandemic. Dr. Robert Garry, a virologist at Tulane School of Medicine, said antibodies should likely protect survivors for several months. Read more...
New Podcast Focuses on COVID Immunity
The “On Good Authority” podcast presents Tulane experts discussing leading issues in the news. The first episode of the podcast features two of Tulane’s most renowned researchers, virologist Robert F. Garry Jr. and immunologist James McLachlan from the School of Medicine, discussing “Is COVID-19 Immunity Possible?”
Be sure to subscribe to On Good Authority, a new Tulane podcast featuring cutting-edge insights from leading experts on global topics. The inaugural episode, “Is COVID-19 Immunity Possible?,” features two of Tulane’s most renowned researchers, virologist Robert F. Garry Jr., PhD, and immunologist James McLachlan, PhD, from the School of Medicine. They will discuss what has been learned about COVID-19 antibodies and why the innate immune system may be more important in fighting off the novel coronavirus than first realized. Read more...
Tulane researchers awarded Fast Grant for second-generation COVID-19 vaccine

Immunologist James McLachlan, PhD, and microbiologist Lisa Morici, PhD, were awarded a Fast Grant for a project to test whether Tulane adjuvants derived from bacteria can make COVID-19 vaccines more effective and longer lasting.==Photo by Cheryl Gerber.
As pharmaceutical firms race to bring the first COVID-19 vaccines to market, scientists are already working on version 2.0. Two Tulane University researchers were awarded a $150,000 Fast Grant for a project to make next-generation COVID-19 vaccines more effective.
Microbiologist Lisa Morici, PhD, and immunologist James McLachlan, PhD, will test whether they can elicit a better immune response in tissues most vulnerable to SARS-CoV-2 infection — the lungs and gut — by adding two bacteria-based adjuvants to COVID-19 vaccines in development. Adjuvants are ingredients used in vaccines to trigger an immune response. Read more...
Tulane receives $2 million to decipher why some asthmatics are highly sensitive to fungi

Chad Steele is professor and chair of the Department of Microbiology and Immunology at Tulane University School of Medicine. (Photo by Paula Burch-Celentano)
The spores that live on everything from carpets to ceiling tiles can cause a severe reaction among the large group of asthmatics who demonstrate sensitivity to fungi. A new Tulane University study aims to discover why this certain group of asthmatics experiences worse asthma, characterized by lower lung function and a more severe allergic reactions, when compared to asthmatics who react to other irritants. Read more...
From Proposals to Funded Research in 48 Hours...

Mairi Noverr of Tulane University School of Medicine along with Monica Vaccari and Tracy Fischer of Tulane National Primate Research Center all received Fast Grants for COVID-19 research.
Three Tulane University researchers are the recipients of new Fast Grants, awards designed to quickly fund COVID-19 related projects. Mairi Noverr, Monica Vaccari and Tracy Fischer received a total of $350,000 for their proposals, all of which progressed from mere proposals to fully funded projects in just 48 hours. Read more about these Tulane Scientists
Trump administration terminates funding of coronavirus bat research in China - CBS News
The Trump administration has cut funding for U.S. nonprofit research into coronaviruses in bats. The renowned EcoHealth Alliance saw its $3.7 grant revoked over their ties to the Wuhan Institute ...
Chad Steele has been named a 2020 Fellow of the American Academy of Microbiology (AAM).

Chad Steele, professor and chair of the Department of Microbiology and Immunology at Tulane University School of Medicine, has been named a 2020 Fellow of the American Academy of Microbiology (AAM). (Photo by Paula Burch-Celentano)

Women respond more vigorously to infection and vaccination compared to men, but they're also more susceptible to autoimmune diseases. James McLachlan, PhD, and his research team at Tulane University School of Medicine launched a new study to find out why. (Photo by Shutterstock)
Physician-Scientist Sets a Course for Fighting Outbreaks
Dr. Sally Baker was one of Tulane’s first public health undergrads (starting the semester Hurricane Katrina hit) and later joined Tulane’s then newly launched MD/PhD physician-scientist program. She recently graduated with MD/PhD degrees. (Photo by Sally Asher)
Tulane PhD Student Wins Regional Three Minute Thesis Competition
Tulane Bioinnovation PhD student Samantha Kurtz won the 2019 Three Minute Thesis Competition with her presentation on her research into novel drug delivery systems to treat early-stage breast cancer. (Photo by Paula Burch-Celentano)
Tulane Awarded $8.5 Million Contract to Develop Next Generation Whooping Cough Vaccine
Tulane researchers James McLachlan and Lisa Morici explain how nanoparticles shed from bacteria can be used in future vaccines to illicit a more potent immune response than existing technologies. Video by Carolyn Scofield and Keith Brannon.
John Clements: A career devoted to lifesaving vaccines

Professor John Clements, PhD, is retiring from Tulane School of Medicine in June, after chairing the Department of Microbiology and Immunology since 1999. Over the past 35 years on the Tulane faculty, he has helped to secure $40 million in grants, including one that paid for five new “ballroom labs” he designed in the J. Bennett Johnston building. After Hurricane Katrina, Clements played an instrumental role leading a team into New Orleans that rescued decades worth of research from Tulane laboratories.
Q. What should we know about the vaccines that you worked on?
What we really work on are things called adjuvants, things you add to vaccines to make them work better. Just think Tony Chachere’s—it makes everything you put it on a little bit better. Well, that’s what adjuvants do, they amplify the body’s immune response to a vaccine’s antigens.
Q. The adjuvants you work on can improve access to vaccines by helping to reduce the amount of antigens needed in vaccines or allowing them to be delivered differently?
Yes. Our primary focus is vaccines against diarrheal diseases for children in developing countries. These diseases do not affect children in developed countries, so they are not attractive targets for large pharmaceutical companies. Along with numerous other organizations, we explore novel ways to develop low-cost, safe, effective vaccines for these children.
Q: I’m told you enjoy mentoring.
Junior investigators are always asking questions that I would not have thought to ask. The answers allowed us to move forward in directions that I would not have moved on my own. Betzi Norton and Jacob Bitoun in our department will continue working on the same things that I’m working on now, in their own way. It’s a natural progression. And because of them, my science won’t end when I retire. That’s a great consolation to me.
This is an excerpt of an article originally published in the Spring 2018 issue of Tulane Med. Continue on to full article.
New research center launched to study Ebola and Lassa survivors

Tulane University virologists are part of a team of researchers working on a new $15 million federally funded project to help eradicate Ebola and Lassa fever by studying in detail how survivors were able to fight off the deadly viruses.
The Scripps Research Institute will lead the effort via the newly created Center for Viral Systems Biology (CViSB), which includes researchers from Tulane University School of Medicine, Kenema Government Hospital in Sierra Leone, the University of California, Los Angeles, the Ragon Institute and the Massachusetts Institute of Technology.
The new project builds on more than a decade of highly collaborative work in Sierra Leone, West Africa, where scientists and local partners have built research facilities and worked with patients.
“Coupling the powerful tools of systems biology research with the resources built up over the past fifteen years in West Africa will allow important advances in our understanding of Ebola and Lassa fever, two of the deadliest diseases known,” said Robert Garry, PhD, co-director of the new center and professor of microbiology at Tulane.
While Ebola virus outbreaks are rare, the 2013–2016 epidemic in West Africa infected more than 15,000 people, killing more than 10,000. Lassa virus causes recurring outbreaks in West Africa, killing thousands of people a year.
“These are very severe diseases, but some people survive. So the simple question is ‘Why?’ How are some people able to fight off the disease, while others are not?” said CViSB co-director Kristian Andersen, PhD, director of Infectious Disease Genomics at the Scripps Translational Science Institute.
Researchers will use genomic analysis and other advanced tools, including physiological measurements, to study individual disease survivors. They will also develop predictive statistical models for identifying critical disease correlates and analyze large-scale data sets to pinpoint causal host-pathogen interactions. By shedding light on the molecular networks that play critical roles in patient outcomes, the research will allow scientists to identify new targets for medicines and vaccines and inform personalized treatment strategies.
“This is different from a lot of research where we are looking at the outbreaks as a whole,” Andersen said. “In this research, instead we’re zooming in on the individual patient to learn how we can best treat and prevent these diseases in the future."
Tulane disease-fighting effort named a 'Best Bet’ for donor support
WATCH: Tulane's proposal for the MacArthur Foundation's 100&Change grant was named a "Best Bet" by one of the nation's leading philanthropic research centers.
A Tulane University proposal to establish a comprehensive system of infectious disease response, from early detection to the development of new treatments, has been named a “Best Bet” by one of the nation’s leading philanthropic research centers.
The Center for High Impact Philanthropy (CHIP), which is widely recognized as a trusted source of knowledge and education to help donors do more good, sees great potential in a Tulane plan to combat infectious diseases, like Ebola and Zika, before they burst onto the world stage in the form of epidemics. The recognition by the University of Pennsylvania-based CHIP shines a light on deserving proposals that the MacArthur Foundation, a leading supporter of nonprofits, cannot fund but hopes others will.
Tulane was one of 1,904 institutions and groups that submitted proposals for the MacArthur Foundation’s 100&Change grant, which awards $100 million to a single project that can make measurable progress toward solving a significant problem. CHIP analyzed MacArthur’s top applications and identified 11 “Best Bets” that didn’t get the big prize but have the greatest potential for impact.
Tulane’s proposal centered on developing processes to quickly respond to emerging disease threats by creating a seamless “detection to production” system.
“Our solution is to establish an efficient and adaptable system able to identify potential infectious disease threats and quickly develop novel diagnostics, therapeutics, and vaccines, which are critical to stopping the spread of diseases in a timely fashion,” John Clements, professor of microbiology and immunology at Tulane School of Medicine, wrote in the grant proposal.
CHIP noted that Tulane’s proposal was a particularly bold idea worth funding given the combined resources of its schools of Medicine, Public Health and Tropical Medicine and Science and Engineering, as well as its National Primate Research Center, Biodiversity Research Center and affiliated clinical trials units. CHIP’s recommendation also highlighted Tulane’s long history of infectious disease research and prevention.
“[Tulane’s] team of scientists from across the university’s multiple schools, and its past involvement in infectious disease prevention represent unique competencies that the team brings,” says CHIP’s Bold Ideas guide. “In addition, Tulane suggests that the processes it develops will be shared and could eventually be replicated at other institutions.”
“If Tulane is successful in streamlining the process of diagnosing and developing treatment and vaccines for infectious disease and minimizing the response time to an outbreak, loss of life could be dramatically reduced.”
If you would like more information about supporting this project, contact Melissa Ereckson at merekson@tulane.edu.
Researchers hunt for Lassa Fever cure
Story by Katy Reckdahl
October 13, 2017
James Robinson and Robert Garry have tracked the Lassa virus for more than a decade.
Twelve years ago, Robert Garry first suggested that his team at Tulane University School of Medicine could unlock the secrets of the mysterious Lassa virus.
Some researchers were skeptical. “They thought it was too difficult,” Garry said.
For starters, the trip from the closest airport to Tulane’s partners at the Kenema Government Hospital in Sierra Leone took 13 hours, driving over treacherously bumpy dirt roads. Tulane would have to draw blood samples from Lassa survivors at a lab in southern Nigeria and the hospital in Kenema, freeze the samples, then keep them frozen for another long bumpy ride and a trans-Atlantic flight to New Orleans.
Once those practical concerns were overcome, Tulane researchers were faced with a virus that science knew very little about in 2005.
“This virus was an enigma,” said Garry’s longtime colleague, Dr. James Robinson, a professor of pediatrics. “We knew it occurred and that people either died or got better.”
“Before we started, no one knew what the proteins of Lassa virus looked like,” said Garry, a professor of microbiology and immunology. “We knew little about how the immune system responded to the virus. And we didn’t know if our tests would work.”
A few years ago, the Tulane team grieved and suffered setbacks after Kenema’s hospital became ground zero for an explosive outbreak of Ebola virus, a highly contagious hemorrhagic fever whose initial symptoms look similar to Lassa in patients. Despite protective gear, 11 of the hospital’s staff were infected; several died, including the chief nurse and the doctor in charge of the Lassa fever program.
This article appeared first in the September 2017 issue of Tulane magazine. Continue to full article.
New drug protects against advanced Lassa fever
September 05, 2017
Story by Keith Brannon
Tulane University School of Medicine virologists Dr. James Robinson (left) and Robert Garry are part of the research team that developed human monoclonal antibodies for a new Lassa fever therapy.
An experimental therapy using cloned antibodies from Lassa fever survivors was 100 percent effective in stopping the progression of the deadly disease in nonhuman primates up to eight days after infection, according to a new study in Nature Medicine.
The research, conducted by a collaborative team led by University of Texas Medical Branch at Galveston, tested Arevirumab-3, a cocktail of human monoclonal antibodies developed by Tulane University and Zalgen Labs LLC.
Lassa fever is a severe and often fatal hemorrhagic illness caused by Lassa virus. It infects more than 300,000 annually. Women and children are in the highest risk groups for the disease, which is often hard to detect in early stages because initial symptoms are similar to the flu and other common illnesses.
“The fact that Arevirumab-3 was 100 percent effective in rescuing primates more than a week after infection with Lassa virus suggests that this therapy may benefit patients with Lassa fever in West Africa, who often present to the clinic at a late stage of disease,” said virologist Robert Garry, professor of microbiology and immunology at Tulane University School of Medicine. “We are accelerating further development of Arevirumab-3 so that this promising treatment can be deployed into clinics where it is needed most.”
This summer, the National Institutes of Health awarded Tulane $5.7 million to further test and refine the antibody-based treatment to get it ready for clinical trials. Tulane was also awarded $6.32 million to develop a Lassa vaccine.
The vaccine will test antibodies that target a recently identified viral surface structure, called the surface glycoprotein, which can block it from infecting a host cell.
Tulane researchers have been studying Lassa in West Africa with a team of collaborators for more than 14 years. They have developed a rapid test to diagnose the disease in the field and spent years collecting blood samples from survivors to identify critical antibodies against the virus.
Tulane University School of Medicine is now a Center of Excellence in the Global Virus Network (GVN)
Tulane University School of Medicine is now a Center of Excellence in the Global Virus Network (GVN), a organization of leading medical virologists from 25 countries decidated to fighting pandemic viral threats through collaborative research, training and advocacy.

Dr. Robert Garry
Dr. Robert Garry, professor of microbiology and immunology, will lead Tulane's GVN Center of Excellence, which will focus on building research capacity to respond to emerging viral threats in West Africa, an area that recently experienced the deadliest outbreak of Ebola.
Tulane also leads the Viral Hemorrhagic Fever Consortium (VHFC), a public-private partnership of scientists who are developing countermeasures, including diagnostics, immunotherapeutics and vaccines, against Lassa virus, Ebola and Marburg viruses, flaviviruses (including Zika virus) and several other high consequence pathogens.
"Given their breadth and deep expertise in viruses, particularly hemorrhagic viruses, Tulane will be an excellent resource for the GVN," said Robert Gallo, GVN co-founder and scientific director. "Bob Garry's ability to establish successful public-private partnerships, such as the VHFC, to help bring lab research to the clinic, particularly in the field of diagnostics, will be a tremendous boost to the GVN."
Garry helped pioneer a rapid test for Ebola and is now working on diagnostics for Zika virus.
"We look forward to joining the GVN so that we can better foster infrastructure development, research, training and education on detection, prevention, amelioration, and treatment of viral hemorrhagic fever viruses targeting both the scientific and general communities," Garry said. "We have a significant presence in West Africa and are pleased to extend our global reach through the GVN."
The GVN is a global authority and resource for the identification, investigation, interpretation, control and suppression of viral diseases posing threats to mankind. It addresses a global need for coordinated virology training, developing scholarly exchange programs for recruiting and training young scientists in medical virology. It also serves as a resource to governments and international organizations seeking advice about viral disease threats, prevention or response strategies.