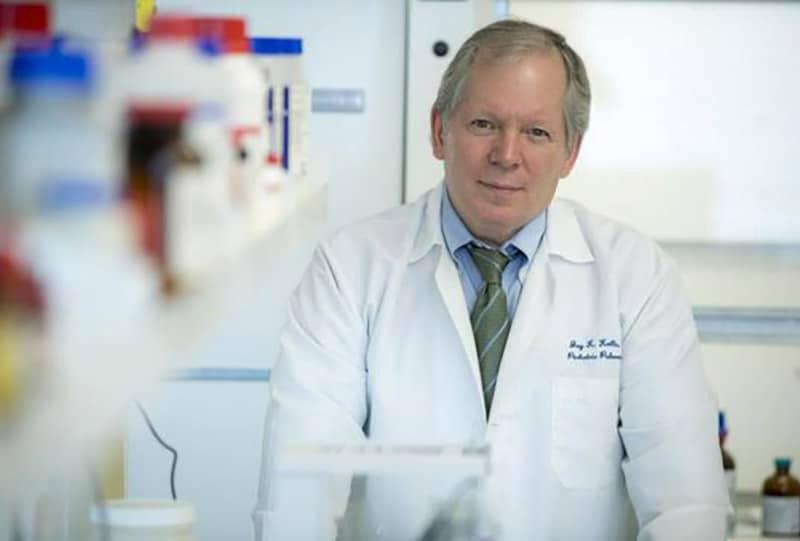
Dr. Jay Kolls Receives Awards for Proposals on Pulmonary Infection
Dr. Jay Kolls has recently received awards for two proposals targeting pulmonary infection.
Immunology of COVID-19
Using a mouse model of SARS-CoV2 infection we are assessing the role of gene modifiers CXCR6 as well as IL-21R signaling in the host immune response to SARS-CoV2. We are testing the efficacy of a mutant ACE2-IgG1 fusion protein has prophylaxis or therapy for COVID-19.
Immunotherapy against multi-drug resistant K. pneumoniae infections.
Carbapenemase producing staining of K pneumoniae (Kpc) are a serious threat to human health particularly in those individuals with underlying diseases such as transplant recipients. We have developed a transplant related model of Kpc infection and using single cell RNASeq to define mechanisms of which calcineurin inhibition, a mainstay of managing transplant rejection inhibits lung immunity against Kpc. With this knowledge we are testing novel host-based immunotherapy to treat these opportunity infections.
These 2 new awards are in addition to 3 ongoing infection-focused pulmonary research grants in Dr. Kolls lab.
CD4+ T-cell Immunity in the Lung
Pneumonia remains the #1 killer of children in the world and is a leading cause of morbidity and mortality in children in the US and the #8 cause of mortality in adults. The research under this R35 investigate CD4+ T cell immunity in the lung and to harness these cells to improve lung resilience against pneumonia.
Improved Therapeutics and Diagnostics for Pneumocystis Pneumonia
This project identifies novel targets to improve treatment outcomes as well as improve diagnostics for PCP particularly in reprice poor settings where bronchoscopy may not be available.
Pathogen Immunity in Cystic Fibrosis
CF is characterized by chronic lung infections. How these impact lung function is determined in part on host immunity. This has been best borne out by assessing host genetics- called gene modifiers which revealed that MHC Class II- the molecule that primes CD4+ T cells. Working with CFFT we have identified a cohort of long term non-progressors and characterize their immune response to P. aeruginosa. Additionally we are validating our human studies in a CF mouse model. Lastly we are studying how S. aureus and P. aeruginosa evade the immune response in CF to persist for decades in the CF lung and sinus.