Annabel Kleess
September 2018
Brief Literature Review
Link to Article: https://tulane.box.com/s/cgcubx8sp4tg27coy4kgh7p7795fcfwi
Open abdominal management after damage-control laparotomy for trauma: A prospective observational American Association for the Surgery of Trauma multicenter study
Summary
Open abdominal (OA) techniques in the setting of severe abdominal trauma have been widely used in the last couple of decades. A decreased risk of abdominal compartment syndrome as well as decreased duration of operation have been cited as prominent benefits among many. This prospective observational study aims to characterize current practices of OA use after trauma and identify independent risk factors that might jeopardize an ideal outcome of definitive primary fascial closure (DPC).
The study enrolled 517 survivors spanning 14 Level 1 trauma centers for two years following a traumatic incident (61% of patients sustained blunt trauma; 84% had a severe abdominal injury). Patients were categorized into those with successful definitive primary fascial closure without complications and those who did not (NPC as in those who died within 48 hours of trauma or who required re-exploration due to complications).
After logistical regression, the study found several independent risk factors that increased the risk of a failed DPC including the number of re-explorations required, development of intra-abdominal abscess/sepsis, bloodstream infection, acute renal failure, enteric fistula and an ISS > 15. Most notably, the increased probability of a failed DPC based on ISS > 15 suggests that there is a relationship between the severity and complexity of initial injury and the probability that the patient will be able to achieve DPC. These patients, in particular, had higher injury severity scores (ISS), blood product requirements, and admission lactate levels and greater blood loss than DPC patients.
Critique This study is an important step in characterizing the current status of managing OA. In its defense, it was a purely observational endeavor and there are an infinite number of variables that could be examined. However, it was noted that 94% of patients received negative pressure wound therapy (NPWT). It is interesting that the paper assessed factors relating to the complexity of the initial injury as well as pathophysiologic processes without controlling for the type/ brand of negative pressure wound therapies used across the study population. Since NPWT was the predominant modality used, future studies might investigate if usage of different types of NPWT is an independent risk factor for failure to achieve definitive primary fascial closure (DPC).
References
Dubose, J. J., Scalea, T. M., Holcomb, J. B., Shrestha, B., Okoye, O., Inaba, K., . . . Ivatury, R. R. (2013). Open abdominal management after damage-control laparotomy for trauma. Journal of Trauma and Acute Care Surgery,74(1), 113-122. doi:10.1097/ta.0b013e31827891ce
Boele van Hensbroek, P., Wind, J., Dijkgraaf, M.G.W. et al. World J Surg (2009) 33: 199. https://doi.org/10.1007/s00268-008-9867-3
Brian Closs, MS Tulane 3
Link to Article: https://tulane.box.com/s/nfjtn8931rd6nnkvdatd63stnzez75fq
Fernando S, Tran A, Cheng W, et al. Necrotizing Soft Tissue Infection: Diagnostic Accuracy of Physical Examination, Imaging, and LRINEC Score; A Systematic Review and Meta-Analysis. Annals of Surgery. 2018
Background
This meta-analysis sought to obtain a summary of diagnostic tests done to evaluate possible necrotizing soft tissue infections (NSTIs) and to evaluate their efficacy. Mortality from NSTIs is estimated to be between 20-30%, with delays to surgical intervention increasing that number. Therefore, it is imperative to have a good understanding of the utility of each diagnostic test. Classical physical exam findings include erythema, soft-tissue edema, severe pain, fever, hemorrhagic bullae, hypotension, and shock. Plain radiographs and CT scans have also been used in the diagnostic process. The Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) score helps to differentiate NSTIs from other soft tissue infections. It consists of the white blood cell count, hemoglobin, sodium, glucose, creatinine, and C-reactive protein, and assigns varying numbers of points for each result. A score greater than 6 indicates a moderate risk and a score greater than 8 indicates a high risk.
Methods
24 cohorts from 23 studies were included in this review. The inclusion criteria for the studies were as follows: 1) enrolled adult patients (≥16 years) with suspected NSTI; 2) conducted in the emergency department, hospital wards, or intensive care unit; 3) evaluated the test characteristics of physical examination, imaging modalities, or LRINEC score for diagnosis of NSTI. Each study was required to have a 2x2 table of true positive, false negative, true negative, and false positive counts, which were either included in the paper or able to be calculated. Bias was assessed using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) tool. Only 3 physical exam findings (fever, hemorrhagic bullae, and hypotension) had at least 3 relevant studies allowing for meta-analysis. Four studies evaluated plain radiography, 7 studied the presence of fascial gas on CT, 14 investigated a LRINEC score >6, and 9 looked at a LRINEC score >8.
Results
Fever had a sensitivity of 46.0% and specificity of 77.0% for diagnosis of NSTI. Hemorrhagic bullae had a sensitivity of 25.2% and specificity of 95.8%. Hypotension was associated with a sensitivity of 21.0% and a specificity of 97.7%. Soft tissue gas on plain radiography had a sensitivity of 48.9% and a specificity of 94.0%. Fascial gas on CT had a sensitivity of 88.5% and specificity of 93.3%. The presence of any one of fascial enhancement, fascial edema, or fascial gas on CT had a sensitivity of 94.3% and specificity of 76.6%. A LRINEC score >6 had a sensitivity of 68.2% and specificity of 84.8%, and a score >8 had a sensitivity of 40.8% and specificity of 94.9%.
Discussion
This review illustrates that the classical description of NSTI as a clinical diagnosis is not supported by the evidence. There were no historical risk-factors suitable for meta-analysis and the only three physical exam findings that were available all had a low sensitivity to detect NSTI. Therefore, they are most likely indicative of more advanced disease. A combination of physical exam findings is more likely to accurately make the diagnosis of NSTI, but none have been evaluated in the literature. On imaging, the presence of fascial gas on CT had a much greater sensitivity and specificity than that of plain radiography. Broadening acceptable CT criteria resulted in an increased sensitivity but a decreased specificity. Similar to physical exam findings, CT findings can encompass a variety of components with differing diagnostic utility. Data is limited or nonexistent on imaging modalities such as MRIs or point-of-care ultrasounds provided only a relatively low sensitivity and moderate specificity. LRINEC >8 increased the specificity but greatly decreased the sensitivity. These results indicate that although the LRINEC is widely used, it has limited efficacy, especially since it may delay definitive surgical management. Individual elements of the LRINEC may actually have better individual accuracy than the LRINEC as a whole. There are several limitations and sources of bias in this review. First, according to QUADAS-2 criteria, 11 studies (47.9%) included in the review had an unclear risk of bias, as they did not mention if the individuals interpreting test results, especially regarding the LRINEC, were blinded to the knowledge of the final diagnosis. Secondly, the studies varied widely in patient selection, with 5 of them considered high risk of bias. Three studies looked specifically at cervical NSTI, which may or may not be applicable to all types of NSTI. One study only included ICU patients and another only included patients with confirmed infection. Additionally, some studies only included patients considered to be high risk (those undergoing imaging or surgery to rule out NSTI), whereas others included all patients with a skin or soft tissue infection. Third, not all hospitals have access to CT imaging and even in those that do, it may delay definitive surgical management, which can lead to increased mortality. Therefore, the utility of this test cannot be based on the sensitivity and specificity alone. Finally, there is also a relative lack of literature published regarding diagnostic tests for NSTI. Only 3 physical exam findings were able to be included, and potentially promising imaging techniques, such as MRI or ultrasound, were unable to be included at all.
Melissa Goldberg (Tulane Third Year Medical Student, Trauma White Surgery Rotation)
Article Review:
Wagner C, Sauermann R, Joukhadar C. Principles of Antibiotic Penetration into Abscess Fluid. Pharmacology 2006;78:1-10
Link to Article: https://tulane.box.com/s/yyp6h7ox3o7ai4c9h751rlnwf1klzx4g
Wagner et. al sought to provide a comprehensive review on the treatment of abscesses using antibiotic therapy. While this is not the gold standard of treatment, patient condition, abscess location, and the ability to perform percutaneous drainage may limit surgical drainage and options, thus it is efficacious to establish alternative means of treatment.
25 publications containing 179 patients were analyzed from 1995-2006 that administered systemic antibiotics alone to treat the abscess (without any surgical intervention). Inclusion criteria included reporting which antibiotic, dosing, duration, and abscess size. Results showed that 88% of cases resulted in clinical recovery or abscess resolution. Abscess size played a role, with significant differences between small and large abscesses (which varied and were not always reported between studies) being reported in the success of treatment within each study. The duration of antibiotic treatment varied from 3 to >360 days and did not seem to play a significant difference in outcomes. These results fall in line with a systematic analysis done by Bamberger that analyzed 138 similar cases between 1966-1994, with an 85% successful treatment rate of abscesses using antibiotic therapy. Again, of the cases that reported abscess size (n= 78 of 465), all that were <5cm were treated successfully with antibiotics alone, with duration of treatment not seeming to play a factor.
Antibiotic concentrations and considerations of the pharmacokinetics and efficacy of antibiotics were also analyzed in rodents and models. Antibiotic penetration into the abscess must cross the capillary endothelium, interstitial space fluid, and abscess membrane using diffusion, permeation, and bulk flow that depend on factors such as lipid-solubility and pH gradients. These studies have shown that Abx penetration is believed to be favored by negligible protein binding and low relative molecular weight.
Pros-This paper concluded that the success of treatment of abscesses with antibiotics is a result of the size of the abscess and the pharmacokinetics of the antibiotics. Small abscesses (with the definition of small varying) may be successfully treated with antibiotic therapy alone, with less importance placed on duration of treatment as compared to the size of the abscess. In addition, the antibiotic chosen having the pharmacokinetics to penetrate into the space is likely to influence outcomes. However, this study has several limitations that must be considered, some of which were addressed by the authors themselves. >
Cons-The publication review done by the authors sustained selection bias in the clinical cases reviewed. By only considering cases that used antibiotic therapy alone, there was no inclusion of abscess conditions that were self-selected to be not-treatable with antibiotics, possibly skewing the results to favor antibiotics when not all cases support this. The outcome variables varied per different reports, with measurements such as abscess size not being uniform, and in some cases not being defined by a concrete number. This calls into question what cutoff can and should be used to qualify what a small abscess, which was the conclusion of what could be successfully treated with antibiotics, is defined by. This limits the application of the results of this study in clinical practice.
It is difficult to measure antibiotic concentrations and activity in humans because individual abscesses can not necessarily be assessed and analyzed at the same time. This paper attempted to apply alternative experiments to get around this. The rodent data showing concentration of antibiotics within abscesses may not be able to be applied to humans, as abscess size varies significantly between the two. The abscess models postulating pharmacokinetics are also theoretical conditions whose practical application in humans would need to be applied before conclusions can be definitively drawn.
Thomas H Fox, Tulane MS 4
BACKGROUND ON THIS STUDY
No study conducted to date has demonstrated improved survival in trauma patients suffering hemorrhagic shock who are treated with REBOA versus resuscitative thoracotomy (RT). In order to evaluate the utility of REBOA and to refine the procedure, the Aortic Occlusion in Resuscitation for Trauma and Acute Care Surgery multi-institutional database (AORTA) was created in 2013. Results from this database failed to show a difference in mortality between the two interventions. Megan Brenner, a surgeon, intensivist and long-time REBOA advocate at Shock Trauma in Baltimore conducted a subgroup analysis using the AORTA database to determine if a difference in outcome between the two approaches could be seen in a select group of patients.
METHODS
Inclusion criteria: Adults undergoing aortic occlusion (AO) in zone 1 of the aorta in the emergency room setting, who did not have penetrating trauma to the thorax. Patients were divided into RT or REBOA based on admitting institutions’ guidelines.
Patients were grouped into three categories: those requiring CPR before hospital admission, after admission but before AO, and those who did not require CPR. The last group was divided into patients who were hypotensive vs normotensive at admission. Patients who went directly to AO after PEA were included in the CPR group.
Primary outcomes between the intervention groups were survival beyond ED and survival to discharge. Secondary outcomes were timed from the beginning of the procedure to AO, adjunctive procedures required, resuscitation requirements, lab values, LOS values for survivors.
RESULTS
285 patients metinclusion criteria over the study period (11/2013-1/2018). 60% of patients (n=172) required CPR before admission, and 20% (n=57) of patients required CPR after admission but before AO. No statistical difference in survival was demonstrated between these groups, and these patients will not be discussed further.
In the remaining 20% (n=56) of patients not requiring CPR before AO:
70% achieved survival beyond the ED(RT: 48%[n=14/29], REBOA: 93%[n=25/27]. P<0.001)
13% survived to discharge(RT: 3.4%[n=1/29], REBOA: 22.4%[n=6/27]. p=0.048).
In patients who were hypotensive (SBP<90) at admission, 65% survived beyond ED, and 15% survived to discharge(RT: 0%[n=0/17], REBOA: 44%[n=4/9]. p=0.008)
DISCUSSION/STUDY BIAS
Results demonstrate that adult trauma patients presenting in extremis who do not require CPR are more likely to survive if treated with REBOA over RT. Bias existed in selecting patients, inpatient characteristics between intervention groups, in trauma center expertise, and in operator experience.
- Patients were grouped into intervention groups based on admitting institutions’ guidelines, and we are not told what those guidelines are.
- Brenner goes out of her way to state that prehospital demographics between the two intervention groups are roughly equivalent (HgB, GCS, age, ISS, admitting SBP). However, SBP at time of AOwas 64 (IQR: 29) in the REBOA group and 0 (IQR: 0) in the RT group. Brenner explains this discrepancy is due to some REBOA group patients having intra-arterial BP monitoring, which is more accurate than a cuff measurement in hypotensive patients. Maybe so, but a 0 value is too low and 64 is too high to explain this discrepancy. Further, the HR measured before AO was 106 +/-34 in the REBOA group and 12 +/-35 in the RT group, indicating that the group undergoing RT were more sickthan those in the REBOA group when they received the AO.
- 94% of patients in the REBOA group received this intervention at one of two trauma centers. Institutions using this cutting edge technology are more likely to deliver higher quality care because they have experience with the technology and with routinely handling trauma patients (eg shock trauma center). I do not have data to support that statement. Those who received REBOA were more likely to receive other adjunctive treatments as well, which may have contributed to their improved survival.
- 94% of REBOA procedures were performed by attending physicians boarded in surgical specialties whereas only 52.8% of RT procedure were performed by attending physicians.
BACKGROUND ON REBOA
REBOA is an acronym for resuscitative endovascular balloon occlusion of the aorta. This procedure is indicated as a temporizing measure to halt hemorrhagic processes occurring distal to the aorta in patients in arrest or extremis, to buy time to get the patient to the operating room and provide definitive treatment. In recent years this process has emerged as a possible alternative to resuscitative thoracotomy (RT) with cross-clamping of the aorta, which is associated with tremendous mortality.
REBOA is performed by placing a balloon in the aorta through a 7F catheter in the common femoral artery (CFA). The CFA is cannulated, a stiff wire inserted and advanced to the second intercostal space, which is confirmed by a chest x-ray. For patients in extremis, it is often difficult to access the CFA through a needle stick, and more than 50% of cases required a CFA cut down for cannulation. A 7F catheter is then placed in the CFA, and the aortic balloon is placed through this catheter and advanced to one of three zones of the aorta. The first zone extends from the origin of left subclavian to the celiac trunk, the second from celiac trunk to renal artery, and the third from renal artery to bifurcation of aorta into common iliacs. The more proximal the balloon, the better probability of stopping the hemorrhage, the greater chances of incurring adverse effects due to lack of perfusion downstream of the occlusion, and the shorter amount of time until those adverse effects occur. No study has been conducted to date that evaluates how long an aortic balloon can be inflated without incurring adverse effects. Anecdotal reports indicate that balloons in zone 1 have remained for up to 90 minutes, while those in zone 3 have remained for up to 5 hours without sustaining adverse effects for the patients. Because of the size of the 12F catheter used for this procedure, a cut down is indicated to remove the catheter. Because of the need for cutdowns both in placing the catheter and removing it, a vascular surgeon is required for placement.
ADDITIONAL INFORMATION ON REBOA IF YOU ARE THIRSTY
Scott Weingart podcasts (1stis interview with Brenner. Second is interview with guy who performed first prehospital REBOA, in a parking lot)
https://emcrit.org/emcrit/reboa/
https://emcrit.org/emcrit/emcrit-podcast-133-first-prehospital-reboa/
Link to REBOA training course (cost: 1500$, must by PGY4 or above): https://www.facs.org/quality-programs/trauma/education/best
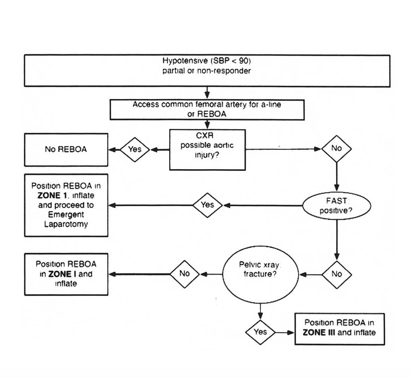
REBOA algorithm from Shock Trauma
Corinne Sommi
Synopsis
7/15/18
Review: Togawa S, Yamami N, Nakayama H, Mano Y, Ikegami K, Ozeki S. The validity of the mangled extremity severity score in the assessment of upper limb injuries. J Bone Joint Surg Br. 2005 Nov;87(11):1516-9
The mangled extremity severity score (MESS) was originally published in 1990 to better select trauma victims whose injured lower extremities warranted primary amputation (1). MESS is based on skeletal/soft-tissue damage, limb ischemia, shock, and age. In the retrospective survey and prospective trial included within the initial article, a MESS calculation greater than or equal to 7 predicted amputation with 100% accuracy (1).
Togawa et al. investigated the validity of MESS applied to the upper extremity in a case series (2). As the scoring system was devised for lower limb trauma, the authors questioned the proper application of MESS to the upper limb. The authors documented the treatment and outcomes of three patients with MESS scores of 7 points or higher, with a range of 7-11 in the selected cases (2). Of the three, one patient underwent upper arm amputation. The patient had a MESS score of 11 and amputation was performed to achieve hemostasis in a situation where the patient could not otherwise be brought out of primary shock. The other two patients had MESS scores of 7 and 11, and both patients’ injured limbs were salvaged. Following multiple surgeries, both patients with salvaged limbs achieved a grade 2 Chen classification, meaning thumb and finger function was restored to where the digits/hand could be used effectively in daily activities (2).
The authors identified ways in which the MESS scoring system did not provide an accurate assessment of the viability of the patients’ limbs (2). In limb injuries, the key reasons to amputate are to avoid infection, crush syndrome, and life-threatening hemorrhage (2). However, the choice to salvage the limb and its success depend upon the skill of the surgeon, which is not included in the MESS criteria. The authors also noted that neither patient with salvaged arms developed crush syndrome, possibly due to the decreased muscle mass in the arm vs. leg and therefore decreased dying muscle tissue (2). The ischemic time for the upper limb is also different than the ischemic time for the lower limb. The maximum time for reperfusion of the arm is eight to ten hours, which falls outside of the six-hour bounds of the MESS score (2). Lastly, the authors pointed out that the chances of limb salvage can be increased through the use of hyperbaric oxygen therapy (2).
MESS also does not include comorbidities such as diabetes mellitus, a known hindrance to wound healing, as well as additional patient injuries suffered in a polytrauma. The MESS score is a valid standard for evaluating lower limb injuries, but based on the findings of Togawa et al. it should be questioned in its application to upper limb trauma.
REFERENCES
- Johansen, K, et. al. Objective criteria accurately predict amputation following lower extremity trauma. Journal of Trauma, 1990.
- Togawa S, Yamami N, Nakayama H, Mano Y, Ikegami K, Ozeki S. The validity of the mangled extremity severity score in the assessment of upper limb injuries. J Bone Joint Surg Br. 2005 Nov
The Bone and Joint Journal
The validity of the mangled extremity severity score in the assessment of upper limb injuries
Therese Nguyen
TUSOM|Class of 2020
Synopsis
A Multicenter Randomized, Controlled Clinical Trial of Transfusion Requirements in Critical Care, also known as the -TRICC trial, investigated whether a restrictive versus liberal transfusion threshold alters mortality in critically ill patients. 838 patients with euvolemia after initial treatment, anemia (hgb concentrations £9 g/dl) within 72 hours of admission to the ICU, and an expected stay in the ICU of ≥ 24 hours where enrolled. Exclusion criteria included: active blood loss, chronic anemia, and admission after routine cardiac surgery. The patients were randomized into the restrictive group that had a target hemoglobin of 7-9 g/dl (transfused if <7 g/dl) and the liberal group that had a target hemoglobin of 10-12 g/dl (transfused if <10 g/dl).
Overall mortality was similar in both groups (18.7% in restrictive group vs 23.3% in the liberal group; P=0.11). Mortality rate was significantly lower in the restrictive approach group in patients that were less acutely ill (APACHE II score £20) and patients younger than 55 years old. There was no significant difference in rates of cardiac events, infectious complications, or multiorgan failure. The authors concluded that red cell transfusion did not offer a survival advantage in euvolemic ICU patients when hemoglobin transfusion thresholds exceeded 7.0 g/dl. The lower threshold offers an inexpensive intervention that improved clinical outcomes and reduced exposure to blood products. There were no significant rates of adverse outcomes in patients with cardiac disease; however, the authors caution the use of the restrictive transfusion strategy in patients with coronary artery disease.
The New England Journal Of Medicine
"A Multicenter, Randomized, Controlled Clinical Trial of Transfusion Requirements in Critical Care"
