New Method Speeds Up Detection of Elusive Lung Infections
A new study from Tulane University School of Medicine introduces a faster, more precise method for identifying infections caused by nontuberculous mycobacteria (NTM)—a diverse group of environmental mycobacteria that can cause opportunistic infections in the lungs and other parts of the body.
NTM are commonly found in water, soil, and dust. They’re usually harmless in healthy people but can cause illness in those with lung problems, weakened immune systems, or medical implants. NTM infections can affect multiple organ systems, most commonly the lungs, but also the skin, lymph nodes, and soft tissues. Diagnosis is often delayed due to the slow growth of these organisms in culture, complicating clinical management and delaying appropriate treatment.
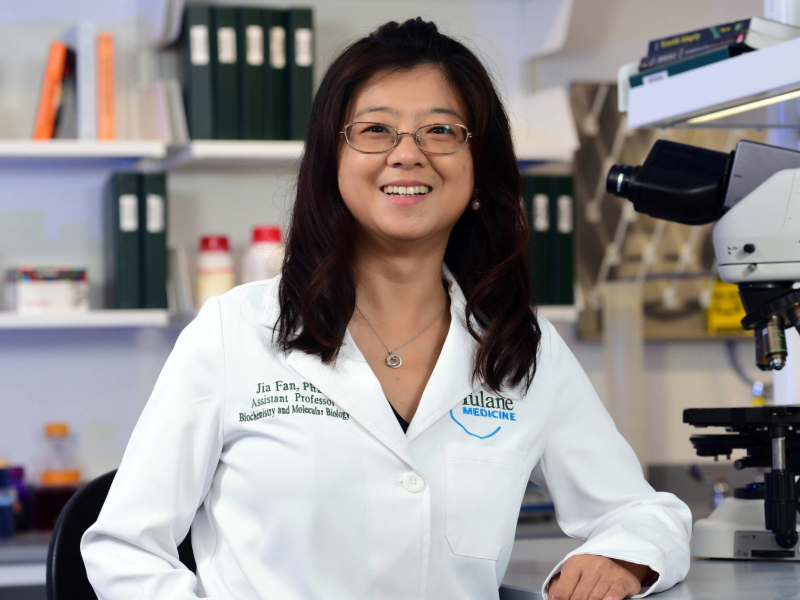
Dr. Jia Fan, assistant professor of biochemistry and molecular biology at Tulane, and her team have developed a novel mass spectrometry-based workflow to improve this process. The method, called PEP-TORCH (PEPtide Taxonomy/ORganism CHecking), integrates optimized sample preparation with a computational algorithm to rapidly and accurately identify NTM species directly from clinical isolates.
The study, published in EMBO Molecular Medicine, demonstrated that the PEP-TORCH workflow identified in more than 100 tested NTM clinical samples down to the species, subspecies, and strain level, surpassing the resolution of conventional diagnostic techniques. A blood test, also developed at Tulane, targets three major NTM species, but this new method has identified more than 200 NTM species.
“This approach significantly reduces the time needed to identify clinically relevant mycobacterial species,” said Dr. Fan. “It provides a reliable alternative to culture and sequencing, which are time-consuming and often lack subspecies-level resolution.”
Unlike conventional diagnostic methods, the PEP-TORCH workflow uses liquid chromatography–tandem mass spectrometry (LC-MS/MS) to detect sequence-specific peptides that are unique to individual mycobacterial taxa. This enables high-resolution identification of closely related species, which is critical for informing species-specific treatment regimens.
In head-to-head comparisons, the new workflow reduced the average time to identification by approximately two weeks. This time-saving has important clinical implications, allowing for more timely and targeted antimicrobial therapy in patients with suspected NTM infections.
The platform also enables the selection of species-specific peptides that can serve as markers for downstream mass spectrometry applications, paving the way for improved quantitative assays and real-time clinical monitoring.
“This is more than just a diagnostic tool,” Dr. Fan noted. “PEP-TORCH provides a flexible framework that can be expanded to other clinically relevant pathogens, especially those that are difficult to culture or distinguish by conventional means.”
The research was supported by the Clinical Center at the National Institutes of Health, which provided well-characterized clinical samples for validation.
As the need for precise and rapid pathogen identification continues to grow, this study highlights the potential of mass spectrometry-based diagnostics to transform the clinical approach to complex infectious diseases.