Residents in training participate in all clinical aspects of our service, including radical and robotic surgeries. In addition, there are ample opportunities to be involved in clinical research.
The Gynecologic Oncology rotation is 4 weeks in length and occurs twice in the PGY2 and PGY4 years. The house officer is responsible for the supervision of the Gynecologic Oncology inpatient service. S/he is either the surgeon or first-assists on appropriate cases. S/he presides over the Gynecologic Oncology clinic where s/he works closely with the Gynecologic Oncology attending. During this rotation s/he takes night call at University Hospital or Tulane-Lakeside where call duties would include coverage for obstetrics and gynecology services.
- Develop core knowledge of critical care for oncology patients
- Diagnosis and treatment of fluid and electrolyte imbalance, cardiac arrest, shock, hemorrhage, multisystem failure and nutritional problems Complex surgical staging procedures
- Complex surgical treatment for gynecological cancer
- Expand core knowledge of:
- Risk factors associated with gynecological malignancies
- Historical and physical findings associated with a gynecological malignancy
- Screening tests for gynecological malignancies
- Embryology, anatomy, histology, and physiology of the female urogential tract, the bowel, and the pelvis
- Vascular, lymphatic and nerve supply to the pelvic organs
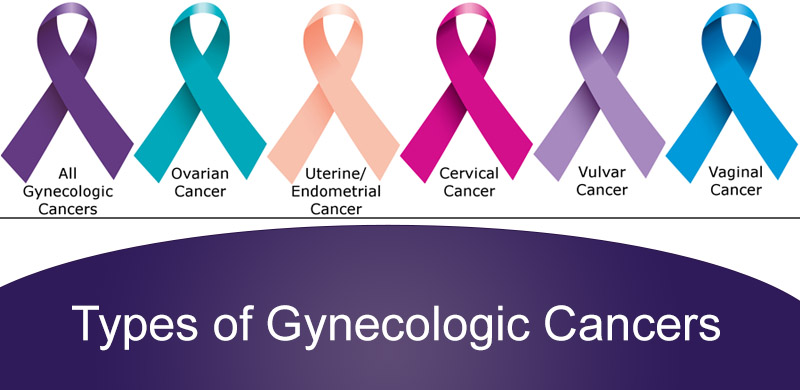
- Gynecological cancer staging
- Surgical treatment for gynecological cancer
- Alterations in immune mechanisms that result from cancer and chemotherapy
- Genetics and how it relates to treatment and inheritance of cancer
- Abdominal surgery principles
- Preoperative evaluation
- Postoperative care
- Intraoperative complications
- Cancer staging of gynecological cancers and correlate stage with prognosis
- Refine surgical skills in the retroperitoneal space
- Identify the ureter from the kidney to the bladder
- Perform:
- Ovarian cancer debulking
- Radical hysterectomy
- Surgery on the vulva/vagina
- Manage intraoperative complications:
- Cystotomy
- Enterotomy
- Hemorrhage
- Manage postoperative complications
- Fistulas
- Pelvic abscess
- Bowel obstruction
- Coordinate critical care for oncology patients
Interpersonal and Communication Skills
- Develop skills in counseling:
- Medical, legal, and ethical implications of "Do not resuscitate" order
- Recognize and know how to deal with the durable power of attorney for patients and the legal rights of this individual
- Counsel patients regarding burial options
- Counsel patient regarding autopsy and understand how to obtain an autopsy consent
- Understand who can consent for an autopsy in this state
- Demonstrate understanding of the unique psychological social, and sexual problems that may arise as the patient and her family cope with gynecological cancer and treatment.
- Demonstrate the ability to support the morale of the patient with compassion and understanding throughout the disease course
- Demonstrate sensitivity when address issues in terminal care
- Provide an adequate sign-out to the on call team to ensure excellent continuity of patient care
- Demonstrate an understanding of the stress, and anxiety of family members who take care of terminally ill patients
- Recognize how family dynamics impact the care of a terminally ill individual
- Develop leadership skills that help your team cope with the stress of taking care of dying patients
- Refine your skills in dealing with difficult patients and family members
- Investigate the impact of palliative care on quality of life
- Investigate psychosocial issues of dying patients
- Use appropriate information resources to identify evidence-based literature, evaluate the quality of data, and apply results to specific patient care issues
- Recognize how long-term health care insurance works
- Recognize the impact the care of the terminally ill patient has on the Medicare budget
- Develop an awareness of how the cost of screening tests compare to the cost of treatment of a cancer patient
- Recognize the importance of GOG protocols
- Recognize the difference between Phase I, II and III trials
- The Obstetrics and Gynecology Library and the Tulane Rudolph Matas Library, and the resident call room have major obstetrics, gynecology, and gynecology-oncology textbooks, journals, instructional videos and access to computers.
- Residents attend Grand Rounds and didactic resident conference
- Attending round on current in-hospital patients.
- Chief Residents' round which occurs twice daily and where short educational presentation are given
- Review of all surgical cases by Chief Resident with all team members weekly prior to surgery day
- Alternating Mondays - Gynecology-Oncology/Pathology Conference: in conjunction with faculty from the Pathology department
- Weekly Tumor Board on Wednesday – multidisciplinary meeting where residents are responsible for case presentations
- Direct verbal feedback is encouraged by the faculty and upper level resident so that resident performance can be commended or improved during the rotation
- Surgical competency is being evaluated with the use of Global rating scale of operative performance. Immediate feed-back is available for the resident to review and discuss with the attending physician
- Residents are evaluated via a Web-based evaluation system at E-Value.com at the end of each rotation using a standardized evaluation form given to supervising Obstetrics and Gynecology attendings. These evaluations are available for immediate review by the resident once completed.
Gynecologic Oncology
Jessica Shank, MD, Section Chief of Gynecologic Oncology
Radiation Oncology
Kendra Harris, MD, Chair of Radiation Oncology
Audrey Dang, MD, Radiation Oncology
Wenzhou Chen, PhD, DABR, Lead Radiation Physicist
Carol Boyd, CMD, Radiation Dosimetrist
Oncologic Fertility
Ronald Clisham, MD, HCLD, Reproductive Endocrinology
Pelvic Floor Disorders
Margie Kahn, MD, Director of Female Pelvic Medicine & Reconstructive Surgery
Cervical and Vulvar Dysplasia
Amber Naresh, MD
Gynecologic Pathology
Lorene Yoxtheimer, MD, Director of Gynecologic Pathology
Genetics
Gabriela Pridjian, MD, Chair of Obstetrics & Gynecology
Chris Dvorak, MS, LCGC, Genetic Counselor
Nikki Walano, MS, LCGC, Genetic Counselor
Interventional Radiology
Brookes Ezell, MD
Bruce Bordlee, MD
James Caridi, MD, FSIR
Gastroenterology
Robin Staudinger, MD
Clinical Psychologist
Aaron Armelie, PhD, Clinical Psychologist
Oncology Nutrition
Michelle Fradella, RD, CSO, LDN
Social Worker
Melissa Barrois, LMSW
Women's Health Lead Nurse
Mayra Gonzalez, RN
Oncology Infusion Team
Missy Bean-Tanner, RN - Supervisor
Amber Hamilton, RN
Bonnie Hunt, RN
Valerie Langford, RN
Heather Monteleone, RN
Heather Zimmerman, RN
Lakeisha Bell - MOA
Oncologic Pharmacy
Queenet Ibekweh, PharmD, BCPs, BCOP, Oncology Pharmacy Coordinator
Hemali Upadhyawa
Carrie Brondum
Financial Counselor
Shawna Blackmore
Medical Office Assistants
Tasha Crutcher
Antoinette Charlot
Quiana Raymond

