Breast cancer is a diagnosis that occurs when a malignant tumor has formed in the breast. Breast Cancer often begins in the ducts or lobules of the breast. Less commonly, breast cancer can begin in the stromal tissues, which include the fatty and fibrous connective tissues of the breast. While breast cancer is the most common cancer in women, it can affect men as well.
Over time, cancer cells can invade nearby healthy breast tissue and make their way into the underarm lymph nodes which are small organs that filter out foreign substances in the body. If cancer cells get into the lymph nodes, this can lead to spread of cancer to other areas of the body. The breast cancer’s stage refers to how far the cancer cells have spread beyond the original tumor.
There are many risk factors for breast cancer. These include, but are not limited to the following:
- Being female (about 100 times more women than men develop breast cancer).
- Older age (the risk of breast cancer rises with age).
- Ethnicity (Caucasian women are at slightly higher risk of developing breast cancer than are African American or Asian women, but African American women are at higher risk of developing triple-negative breast cancer, a specific subtype of the disease).
- History of breast cancer or prior treatment with radiation therapy to the breast/chest in childhood or early adulthood.
- Consuming more than two alcoholic drinks per day on a regular basis.
- Dense breast tissue (women with dense as opposed to fatty breast tissue are at a higher risk of developing breast cancer).
- Early menstruation or late menopause.
- Exposure to certain drugs, including DES, Hormone Replacement Therapy (HRT) and certain other medications.
- History of lobular carcinoma in situ (LCIS), atypical ductal or lobular hyperplasia and other specific conditions identified on breast biopsies (these non-cancerous conditions can suggest a higher risk of developing breast cancer).
In addition to risk factors associated with lifestyle and environmental exposures, there are breast cancer risk factors that occur in families. Certain genetic markers have been identified which, if present, may significantly increase your personal risk of breast cancer. Tulane Cancer Center is able to refer you for genetic counseling with a certified genetics counselor should you report family history of breast or ovarian cancer in your family and it is determined with your physician. Genetic testing analyzing the BRCA1 and BRCA2 genes and other breast cancer-associated genes is performed, as appropriate.
Staging
A staging system is a standardized way for the cancer care team to summarize information about how far a cancer has spread. The most common system used to describe the stages of breast cancer is the American Joint Committee on Cancer (AJCC) TNM system.
Your physicians will use information from physical exam, biopsy, imaging studies and results from surgery to determine staging. Pathological staging is staging made from tests and surgery results. Clinical staging is staging based on exam, biopsy and imaging results.
For a comprehensive guide to staging please see Staging.
How is breast cancer diagnosed?
Diagnostic imaging
Your diagnostic tests may include one or more of the following procedures:
- Mammogram: X-ray images of the breast. The use of digital mammograms provide a clear two -dimensional image highlighting unusual structures such as calcifications or masses, which may need further evaluation.
- Tomosynthesis: 3D digital imaging that uses compression and X-rays; it feels similar to a mammogram, but takes extra images to allow doctors to examine each layer of the breast. Tomosynthesis may increase doctors' ability to find some cancers while also lowering the risk of false positive evaluations; however, it may also expose a person to additional radiation.
- MRI (magnetic resonance imaging): Imaging that may show abnormal tissue more clearly than a mammogram. MRIs are used in special situations, often for individuals who have a genetic predisposition to breast cancer or unclear mammograms.
- Ultrasound: Imaging that can capture the size and structure of a potential tumor. Ultrasound is rarely used for cancer screening because not all cancers are visible on ultrasound. However, in conjunction with mammography, it is a highly useful tool for diagnosis An ultrasound can further characterize an abnormality seen on a mammogram, or help guide the needle during a breast biopsy.
In some cases, more extensive imaging may be necessary to determine whether breast cancer has spread beyond the breast. When this is the case, CT scans and/or bone scans may be used. In select cases, a PET scan may also be necessary.
General types of treatment for breast cancer
The main types of treatment for breast cancer are:
- Surgery
- Radiation therapy
- Chemotherapy
- Hormone therapy
- Targeted therapy
- Bone-directed therapy (bisphosphonates and denosumab)
Treatments can be grouped based on how they work and when they are used.
Local versus systemic therapy
Local therapy is intended to treat a tumor at the site without affecting the rest of the body. Examples of local therapy are surgery and radiation therapy.
Systemic therapy refers to drugs which can be given by mouth or directly into the bloodstream to reach cancer cells anywhere in the body. Chemotherapy, hormone therapy, and targeted therapy are systemic therapies.
Therapies are classified as Adjuvant or neoadjuvant therapy:
Patients who have no detectable cancer after surgery are often given additional treatment to help keep the cancer from coming back. This is known as adjuvant therapy.
This is to avoid the potential risk of any breast cancer cells moving from the original location and spreading to other areas of the body. The goal of adjuvant therapy is to kill these hidden cells. systemic therapy (like chemotherapy, hormone therapy, and targeted therapy) and radiation can be used as adjuvant therapy.
Some patients are given treatment, such as chemotherapy or hormone therapy, before surgery. The goal of this treatment is to shrink the tumor in the hope it will allow a less extensive operation to be done. This is called neoadjuvant therapy. Many patients who get neoadjuvant therapy will not need adjuvant therapy.
Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer.
When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Standard treatments
Surgery - Most patients with breast cancer have surgery to remove the cancer from the breast. Lymph nodes are also removed under the arm and looked at under a microscope to see if they contain cancer cells. Having a sentinel node biopsy at the time of surgery is standard of care. If cancer cells are seen in the sentinel node the surgeon may determine that more lymph nodes under the arm should be removed for evaluation.
Breast-conserving surgery, an operation to remove the cancer but not the breast itself, includes the following:
- Lumpectomy: Surgery to remove a tumor(lump) and a small amount of normal breast tissue around it.
- Partial mastectomy: Surgery to remove the part of the breast that has cancer and some normal tissue around it. The lining over the chest muscles below the cancer may also be removed.
Other types of surgery include the following:
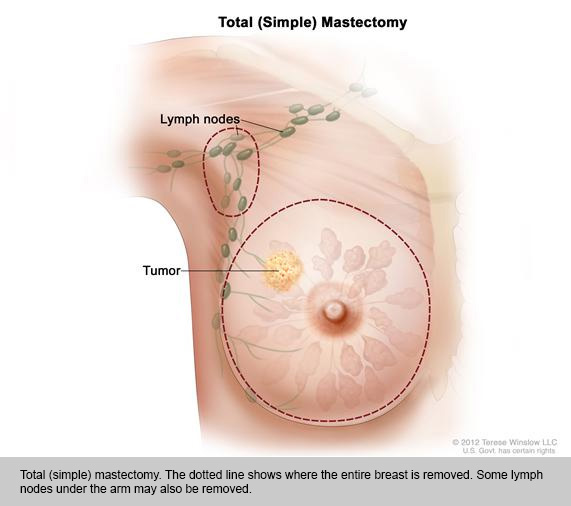
- Total mastectomy: Surgery to remove the whole breast that has cancer. This procedure is also called a simple mastectomy.
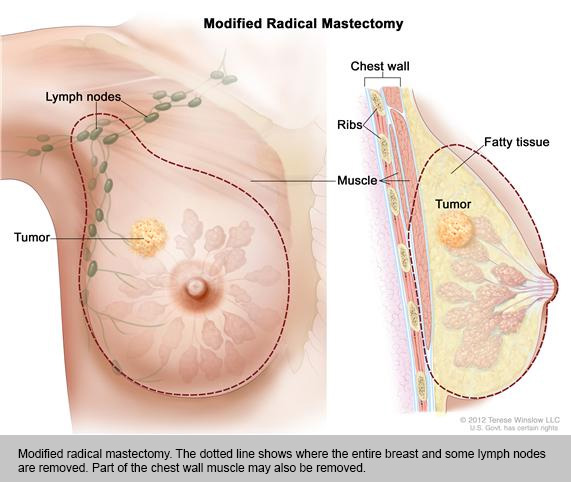
- Modified radical mastectomy. Surgery to remove the whole breast that has cancer, many of the lymph nodes under the arm, the lining over the chest muscles, and sometimes, part of the chest wall muscles.
Chemotherapy and targeted therapy
In most cases (especially adjuvant and neoadjuvant treatment), chemo is most effective when combinations of more than one drug are used. Many combinations are being used, and it's not clear that any single combination is clearly the best. Clinical studies continue to compare today's most effective treatments against something that may be better.
Chemotherapy regimens are usually given in cycles, with each period of treatment followed by a rest period to give the body time to recover from the effects of the drugs. Chemo begins on the first day of each cycle, but the schedule varies depending on the drugs used.
The side effects of chemo depend on the type of drugs, the amount taken, and the length of treatment. Some of the most common possible side effects include:
- Hair loss
- Mouth sores
- Loss of appetite or increased appetite
- Nausea and vomiting
- Low blood cell counts
Chemo can affect the blood forming cells of the bone marrow, which can lead to:
- Increased chance of infections (from low white blood cell counts)
- Easy bruising or bleeding (from low blood platelet counts)
- Fatigue (from low red blood cell counts and other reasons)
These side effects are usually short-term and go away after treatment is finished. It's important to tell your health care team if you have any side effects, as there are often ways to lessen them. For example, drugs can be given to help prevent or reduce nausea and vomiting.
Radiation therapy
Cells that might remain after surgery, to shrink large tumors before an operation so that they can be removed more easily, or to relieve symptoms of Breast cancer Radiation therapy is treatment with high-energy rays or particles that destroy cancer cells. Radiation to the breast is often given after breast-conserving surgery to help lower the chance that the cancer will come back in the breast or nearby lymph nodes. Radiation may also be recommended after mastectomy in patients with either a cancer larger than 5 cm, or when cancer is found in the lymph nodes.
Two types of radiation
External beam - the most common type of radiation therapy for women with breast cancer. The radiation is focused from a machine outside the body on the area affected by the cancer.
The area of radiation and the extent of radiation depends on the type of surgery done and whether lymph nodes were involved. If Cancer was found in the lymph nodes under the arm, radiation may be given to this area as well In some cases, the area treated may also include supraclavicular lymph nodes (nodes above the collarbone) and internal mammary lymph nodes (nodes beneath the breast bone in the center of the chest).
If done post surgery Radiation will usually be initiated after the tissue has time to heal. If chemotherapy is needed as part of the treatment protocol,radiation is usually begins when chemotherapy is complete. Breast radiation is most commonly given 5 days a week (Monday thru Friday) for about 5 to 6 weeks.
Brachytherapy
Brachytherapy, also known as internal radiation, is another way to deliver radiation therapy. Instead of aiming radiation beams from outside the body, radioactive seeds or pellets are placed into the breast tissue next to the cancer. It is often used in patients who had Breast conserving surgery as a way to add an extra boost of radiation to the tumor site (along with external radiation to the whole breast). It may also be used by itself (instead of radiation to the whole breast). Tumor size, location, and other factors may limit who can get brachytherapy.
Targeted drug therapy
As researchers have learned more about the gene changes in cells that cause cancer, they have been able to develop newer drugs that specifically target these changes. These targeted drugs work differently from standard chemotherapy (chemo ) drugs. They often have different (and less severe) side effects. They are most often used along with chemo at this time.
Trastuzumab (Herceptin)
Pertuzumab (Perjeta™)
Lapatinib (Tykerb)
Everolimus (Affinitor®)
Bevacizumab (Avastin®)
Drugs that target specific defects that allow cancer cells to proliferate are available.
Hormone therapy for breast cancer
Hormone therapy is another form of systemic therapy. It is most often used as an adjuvant therapy to help reduce the risk of the cancer coming back after surgery, but it can be used as neoadjuvant treatment, as well. It is also used to treat cancer that has come back after treatment or has spread.
Estrogen promotes the growth of about 2 out of 3 of breast cancers— those having receptors for the hormones estrogen (ER-positive cancers) and/or progesterone (PR-positive cancers). Because of this, several approaches to blocking the effect of estrogen or lowering estrogen levels are used to treat hormone receptor-positive breast cancers. Hormone therapy does not help patients whose tumors are both ER- and PR-negative.
Tamoxifen and toremifene (Fareston®): These anti-estrogen drugs work by temporarily blocking estrogen receptors on breast cancer cells, preventing estrogen from binding to them. They are taken daily as a pill.
For women with hormone receptor-positive cancers, taking tamoxifen after surgery for 5 years reduces the chances of the cancer coming back by about half and helps patients live longer.
Tamoxifen can also be used to treat metastatic breast cancer, as well as to reduce the risk of developing breast cancer in women at high risk.
Aromatase inhibitors (AIs): Three drugs that stop estrogen production in post-menopausal women have been approved to treat both early and advanced breast cancer: letrozole (Femara®), anastrozole (Arimidex®), and exemestane (Aromasin®). They work by blocking an enzyme (aromatase) in fat tissue that is responsible for making small amounts of estrogen in post-menopausal women. They cannot stop the ovaries of pre-menopausal women from making estrogen, so they are only effective in women whose ovaries aren’t working (like after menopause). These drugs are taken daily as pills. So far, each of these drugs seems to work as well as the others in treating breast cancer.
Fulvestrant (Faslodex®): Fulvestrant is a drug that also acts on the estrogen receptor, but instead of just blocking it, this drug also eliminates it temporarily. It is often effective even if the breast cancer is no longer responding to tamoxifen. It is given by injection once a month.. It is currently only approved by the FDA for use in post-menopausal women with advanced breast cancer that no longer responds to tamoxifen .
Megestrol acetate: Megestrol acetate (Megace®) is a progesterone-like drug used as a hormone treatment of advanced breast cancer, usually for women whose cancers do not respond to the other hormone treatments. Its major side effect is weight gain, and it is sometimes used in higher doses to reverse weight loss in patients with advanced cancer. This is an older drug that is no longer used very often.
Ovarian ablation: In pre-menopausal women, removing or shutting down the ovaries, which are the main source of estrogens, effectively makes the woman post-menopausal. This may allow some other hormone therapies to work better. This is most often used to treat metastatic breast cancer.
Permanent ovarian ablation can be done by surgically removing the ovaries. This operation is called an oophorectomy. More often, ovarian ablation is done with drugs called luteinizing hormone-releasing hormone (LHRH) analogs, such as goserelin (Zoladex®) or leuprolide (Lupron®). These drugs stop the signal that the body sends to ovaries to make estrogens. They can be used alone or with tamoxifen as hormone therapy in pre-menopausal women. They are also being used along with aromatase inhibitors in studies of pre-menopausal women.
Bisphosphonates for breast cancer
Bisphosphonates are drugs that are used to help strengthen bones and reduce the risk of fractures and pain in bones that have been weakened by metastatic breast cancer. Examples include pamidronate (Aredia®) and zoledronic acid (Zometa®). They are given intravenously (IV).
Bisphosphonates may also help against bone thinning (osteoporosis) that can result from treatment with aromatase inhibitors or from early menopause as a side effect of chemotherapy. There are a number of medicines, including some oral forms of bisphosphonates, to treat loss of bone strength when it is not caused by cancer spread to the bones.
Denosumab for breast cancer
A newer drug called denosumab (Xgeva®, Prolia®) is also now available to help reduce the risk of problems from breast cancer metastasis to the bone. It works differently from bisphosphonates.
In studies of patients with breast cancer that had spread to the bone, it seemed to help prevent problems like fractures (breaks) better than zoledronic acid (Zometa). It also can help bones even after bisphosphonates stop working.
Lymphedema
Lymphedema is the build-up of fluid in soft body tissues when the lymph system is damaged or blocked.
Lymphedema occurs when the lymph system is damaged or blocked. Fluid builds up in soft body tissues and causes swelling. It is a common problem that may be caused by cancer and cancer treatment. Lymphedema usually affects an arm or leg, but it can also affect other parts of the body. Lymphedema can cause long-term physical, psychological, and social problems for patients.
Possible signs of lymphedema include swelling of the arms or legs.
Other conditions may cause the same symptoms. A doctor should be consulted if any of the following problems occur:
- Swelling of an arm or leg, which may include fingers and toes.
- A full or heavy feeling in an arm or leg.
- A tight feeling in the skin.
- Trouble moving a joint in the arm or leg.
- Thickening of the skin, with or without skin changes such as blisters or warts.
- A feeling of tightness when wearing clothing, shoes, bracelets, watches, or rings.
- Itching of the legs or toes.
- A burning feeling in the legs.
- Trouble sleeping.
- Loss of hair.
Daily activities and the ability to work or enjoy hobbies may be affected by lymphedema.
Cancer and its treatment are risk factors for lymphedema.
Lymphedema can occur after any cancer or treatment that affects the flow of lymph through the lymph nodes. This can happen after the removal of lymph nodes. It may develop within days or many years after treatment. Most lymphedema develops within three years of surgery. Risk factors for lymphedema include the following:
- Removal and/or radiation of lymph nodes in the underarm, groin, pelvis, or neck. The risk of lymphedema increases with the number of lymph nodes affected. There is less risk with the removal of only the sentinel lymph node (the first lymph node to receive lymphatic drainage from a tumor).
- Being overweight or obese.
- Slow healing of the skin after surgery.
- A tumor that affects or blocks the left lymph duct or lymph nodes or vessels in the neck, chest, underarm, pelvis, or abdomen.
- Scar tissue in the lymph ducts under the collarbones, caused by surgery or radiation therapy.
- Lymphedema often occurs in breast cancer patients who had all or part of their breast removed and axillary (underarm) lymph nodes removed.
Tulane has a lymphedema clinic for the treatment of patients with Lymphedema. This is located in our physical therapy department and patients work directly with Certified Lymphedema physical therapists who evaluate, treat and educate patients to manage lymphedema.
For information on the treatment program: please contact
The Physical and Occupational therapy department at Tulane University 504-988-5194
For more information regarding breast cancer and treatment go to:
http://www.cancer.org/cancer/breastcancer/index
http://www.cancer.gov/cancertopics/types/breast http://www.breastcancer.org/
http://ww5.komen.org/breastcancer/understandingbreastcancer.html
